So today’s newsletter is a little different than previous ones – it is less about my personal journey but rather about a common problem a number of patients and caregivers face. The reason it personally resonates with me is that this is one of the hard things about the cancer experience that really should not be this hard! As a scientist, I understand why clinical trials exist, the importance of them for me as a patient, and the value they bring to developing safe and effective treatments. As a caregiver or a patient, finding and enrolling in a relevant clinical trial is still complicated. To put this in perspective, repeated studies have estimated that <5% of adult cancer patients enroll in clinical trials, even though 70% of Amercins say they are very willing/inclined to do so (Source: Study published in ASCO).
Just a reminder: No one sponsors our newsletters. This is not marketing material, and we are not promoting any specific pharmaceutical company or trial.
Let’s get to it.
What is a clinical trial?
Clinical trials are research studies performed with people (i.e., us). These studies are the primary way that researchers find out whether a new drug, diet, or device is both safe and effective in people. Before the U.S. Food and Drug Administration (FDA) approves a clinical trial to begin, they require scientists to have performed a number of studies in the lab and in animals to test whether the treatment is safe and efficacious before they provide their approval to be tested in humans. Based on the results of the many phases of clinical trials, the FDA will approve (or not approve) the drug, diet, or device to enter the market. (Source: NIH)
Why should we care?
As patients, survivors and caregivers we really should care about clinical trials.
- Clinical trials are necessary before we get any new drug or test: For us to get new treatments, new doses, new diagnostics and new screening methods, they first have to successfully pass a rigorous standard of testing through clinical trials. Since 2000, the number of clinical trials that investigate cancer treatments has nearly quadrupled. In 2021, there were 1489 clinical trials in the US (Source: CenterWatch).
- Accessing the newest, most innovative cancer treatments: Some of the newest treatments are only available through clinical trials. The cancer research space changes every few months, and in order to get the latest treatment, you will often need to enroll in a clinical trial. As an example, in my case, I received Herceptin, a targeted treatment for Her2+ breast cancer. This meant that I needed to go in for infusions every 3 weeks for over 19 months. Herceptin itself wasn’t too terrible, but by my 15th cycle, going into the infusion center became pretty emotionally exhausting. My oncologist suggested that I might enroll in a local clinical trial where they were offering Herceptin in a different format that I could take at home. Sadly with covid, it was more convenient to stick it out with the traditional infusion.
- It can be an option when standard of care is not an option: For many in our community who are grappling with metastatic disease, rare cancers, incurable cancers and cancers that have progressed, standard of care may no longer provide a viable option. The National Comprehensive Cancer Network (NCCN) set the standard of care for oncology worldwide. You can listen to the Executive Director of the NCCN on our podcast episode talk about guidelines and understanding standard of care. However, sometimes the standard of care isn’t enough. In these situations, clinical trials can sometimes provide an option. Paula Kim, the co-founder of PanCan and a caregiver herself, speaks about how this was true in her father’s case.
In order to figure out whether you should/should not be looking for a clinical trial, please speak with your oncology care team.
Okay, so, how do you find a clinical trial?
Here’s where life gets a little hard. Today, finding clinical trials that are relevant for your specific case is a hands-on process and sometimes takes a fair bit of work.
- Start by talking to your doctor. If you are getting care at an AMC, an “Academic Medical Center,” they often have clinical trials running at those centers. If you are getting care at a local hospital, your care team might be able to find you a trial near where you are getting treated.
- Look on clinicaltrials.gov. This website is maintained by the US government and lists all trials that are happening and have happened. It is a public repository and is free. It does require a little bit of work. You can look for trials that are “actively enrolling” and reach out to the trial staff directly. If you find a trial on clinicaltrials.gov but cannot figure out how to reach out to them, you might want to take the name of the trial to your oncologist. They might know someone on the research team.
- A lot of new companies have cropped up to help us (patients and caregivers) find clinical trials. We looked at a number of them, and decided to partner with Curia. Curia has taken the information from clinicaltrials.gov and made it much easier to search and find applicable trials. You can download their app and use it for free. NOTE - Please do your own research on these companies. There are quite a few out there. This is simply a starting point that we found based on our own experiences.
If you are still struggling, feel free to reach out to us, and we’d be happy to give you any support we can.
Alright, you found one, now what?
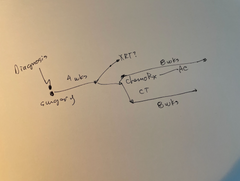
You will need to reach out to the recruiting team. They will typically speak with you, tell you about the trial’s risks and benefits, and what you might expect. A lot of trials are randomized clinical trials, which means that the trial participant could be assigned to a “control” arm or the “experimental” arm. Control arms are created to develop the “baseline” to which you compare the treatment to. The control arm often gets a placebo and/or the standard of care. The experimental arm received the “intervention” that is being studied. You won’t know until you are enrolled in the trial. This is only one type of study, and study designs vary greatly based on what is being tested.
If it’s that straightforward, why aren’t more patients enrolled in clinical trials?
This brings us back to why I’ve been wanting to write about this topic. There is quite a bit of industry knowledge on “patient recruiting” and the many reasons why it is very difficult. In my personal case, the trial timing, covid-19 and being exhausted from my treatment became the reasons I never enrolled in a trial. Studies show that patients are sometimes uneasy about the potential toxic effects of experimental treatments and by the time they get to know about a trial they have already decided on a treatment path. One of the reasons that makes me a little dejected is that some trials require more effort and more frequent monitoring. This can often add a fair amount of burden - getting to/from the cancer clinic, and additional costs associated with partaking in a trial. Even though a majority of states mandate that insurers cover the routine costs of a trial, cost concerns are meaningful. (Source: ASCO study).
Even though I personally did not partake in a clinical trial, I am incredibly grateful to all those women who did take part in the trials that approved the drugs I was given. Without the women who took a risk and enrolled in trials, such as the Phase 3 Herceptin trial, I would never have gotten Herceptin. To them, I am grateful.
If you like this type of information, please respond to us. We tailor a lot of our content based on your feedback.