Introduction
When undergoing breast cancer treatment, there are so many changes to navigate, both physically and emotionally. One of the often-overlooked side effects involves changes to your nails and skin. These changes can feel discouraging or frustrating, but understanding what to expect and how to care for your nails during this time can make a difference. This post will share practical tips, explain why these changes happen, and help you care for your nails and skin during treatment.
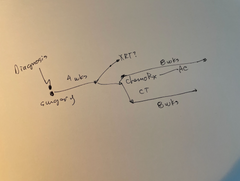
Want more information about symptoms and side effects of cancer treatment? Want to connect with support to help you through the cancer experience? Click here to learn more about Your Interactive Cancer Maps, our step-by-step guide to help you navigate the cancer experience and find the support your need from diagnosis to living with “the new normal” after treatment. Learn more here.
Common Nail Changes Caused by Cancer Treatments
Cancer treatments like chemotherapy and targeted therapy can cause significant changes to your nails. Some of the most common nail issues include:
- Nail Discoloration: Your nails may turn yellow, darken, or even develop a bluish tint. This is a common reaction to the medications used in treatment.
- Brittle or Fragile Nails: Nails may become weaker, prone to cracking, or peeling. Everyday activities like opening a jar or even typing might suddenly feel challenging.
- Ridges and Grooves: Vertical or horizontal lines can appear on your nails, marking the stress your body is undergoing.
- Nail Bed Infections: Inflammation, redness, or pus around your nail beds can develop, especially if the immune system is suppressed.
These changes vary from person to person and depend on the specific type of treatment you are undergoing. Recognizing these changes as part of the process can help you take proactive steps to manage them.
Why Nail Changes Occur
Cancer treatments are designed to target rapidly dividing cancer cells, but they can also affect other fast-growing cells, including those in your nails and hair.. Here are some reasons these changes happen:
- Impact on Cell Growth: Chemotherapy disrupts the growth cycle of cells, including nail cells, which can result in discoloration, ridges, or fragility. Nail cells start and stop growing with each chemotherapy cycle. This process can result in lines on your nails, similar to the rings on tree stumps, which result after tree growth slows during dry times of each year.
- Immune System Suppression: Treatments may weaken your immune system, making it harder for your body to fight off infections, including those around your nails.
- Dehydration and Nutrient Deficiency: Some treatments can deplete your body of vital nutrients and moisture, leading to drier, weaker nails.
Understanding the cause of these changes can make it easier to focus on solutions and give yourself grace during this time.
Preventive Measures and Nail Care Tips
Taking care of your nails during cancer treatment doesn’t have to be complicated. A little extra attention can go a long way in maintaining nail health and reducing discomfort.
Daily Nail Care Routine
- Keep Nails Clean and Trimmed: Regular cleaning and trimming can prevent bacteria from building up and reduce the risk of infections.
- Moisturize Regularly: Use a gentle moisturizer on your cuticles and nails to combat dryness and brittleness. Look for creams or oils that are free from harsh chemicals.
Products to Use
- Non-Toxic Nail Polish: If you want to paint your nails, opt for non-toxic, water-based polishes that are less likely to cause further damage.
- Acetone-Free Removers: When removing nail polish, use acetone-free products to avoid excessive drying and irritation.
Protective Practices
- Avoid Biting Nails: This can introduce bacteria to already sensitive areas.
- Wear Gloves: Protect your hands when doing chores like washing dishes or gardening to minimize exposure to chemicals and dirt.
- Well fit shoes: Shoes that are too tight, or “only hurt sometimes” can damage toenails. The damage won’t heal as quickly during cancer treatment. A good rule is if your feet hurt, then stop – either sit down or wear more comfortable shoes.
Dietary Support
- Biotin-Rich Foods: Incorporate foods like eggs, nuts, and seeds, which are rich in biotin to promote nail health.
- Omega-3 Fatty Acids: Found in salmon, walnuts, and flaxseeds, these nutrients can help improve overall nail and skin health.
Home Remedies
- Natural Oils: Coconut oil or almond oil can deeply hydrate nails and cuticles, making them less brittle.
- Tea Tree Oil: This natural antiseptic can be applied (diluted) to mild nail infections to prevent them from worsening.
When to Consult a Doctor
Sometimes, even with the best care, nail changes may require medical attention. Keep an eye out for the following signs:
- Severe Pain or Swelling: Pain around the nail beds or visible swelling may indicate a serious infection.
- Persistent Infections: If redness, pus, or other symptoms of infection don’t improve, reach out to your cancer care team.
- Nails Detaching from Nail Beds: This can sometimes happen and should be evaluated by a medical professional to rule out complications.
Early intervention can prevent small issues from turning into larger problems. Don’t hesitate to bring up nail concerns with your doctor; they are there to help you feel as comfortable as possible during treatment.
Cancer Maps to help you find your way, one decision at a time.Built for Patients, by Patients. Backed by World-Leading Oncologists

Join a community of people who “get it”
The Manta Cares team is composed of cancer survivors, caregivers, oncologists and nurses - so we truly understand the challenges that come with a cancer diagnosis because we’ve been there. We are here to walk with you as you go through your own cancer experience. Please don’t hesitate to reach out with any questions. We have even developed Your Interactive Cancer Maps, a platform with disease-specific step-by-step maps to show you all the paths you might face during your cancer experience, future treatment options and connect you with relevant support and resources. Sign up for access to the Your Interactive Cancer Maps platform here.
Be sure to subscribe to our newsletter and check out our free resources like our Chemotherapy Checklist for Caregivers, Financial Checklist for Cancer Treatment and more. We also put out a bi-weekly podcast called the Patient from Hell to educate, empower and hopefully inspire you as you go through this crappy experience. You can listen on Spotify, Apple Podcasts, YouTube or anywhere you listen to podcasts. Dealing with cancer as a patient or caregiver can feel really lonely. Just know that you are not alone in this experience.
Also Read:
- Why Do Aromatase Inhibitors Cause Insomnia?
- Importance of Wearing a Compression Bra After Breast Surgery
- 5 Dental Side Effects Of Tamoxifen, Chemo and Bone Drugs
- How to Sleep with a Chemo Port
- Taking A Break From Tamoxifen: When, Why and What To Expect
- Can Claritin Help With Joint Pain From Breast Cancer Treatment?
Conclusion
Changes to your nails and skin during breast cancer treatment can feel like one more thing to deal with, but they are manageable with the right care. By keeping your nails clean, hydrated, and protected, and by recognizing when to seek help, you can minimize the discomfort and protect your nail health. Remember to be patient with your body; it’s working hard to heal.
If you’re feeling unsure or overwhelmed, your medical team is a great resource for advice and guidance. You’re not alone in this, and there are solutions to help you feel more in control.
FAQs on Managing Nail and Skin Health During Cancer Treatment
Q: Does breast cancer affect your nails?
Ans - Yes, breast cancer treatments, especially chemotherapy, can cause nail changes such as discoloration, brittleness, and infections. These changes are usually temporary, and your nails will return to normal after the chemotherapy is stopped or changed.
Q: Does cancer treatment affect your nails?
Ans - Yes, treatments like chemotherapy and targeted therapies can impact the growth and strength of your nails.
Q: What happens when you finish breast cancer treatment?
Ans - Your nails may gradually recover after treatment ends, but it can take several months for them to return to normal.
Q: What skin changes occur due to breast cancer?
Ans - Skin changes can include dryness, sensitivity, or discoloration, often as a side effect of treatments.
Q: How long after chemo will my nails recover?
Ans - Recovery time varies, but nails often start to improve within a few months after treatment ends.
Q: Can breast cancer affect fingers?
Ans - The treatments for breast cancer can affect the nails and skin on your fingers, causing issues like brittleness and infections.
Q: What are the late effects of radiation for breast cancer?
Ans - Radiation can lead to skin dryness, thickening, or sensitivity even months after treatment has concluded. Sometimes, years after breast radiation therapy, prominent small red blood vessels appear and do not go away. These are known as “telangiectasia” and are usually not a cause for concern, unless skin breakdown or lumps occur. Show the skin changes to your cancer care team, either in person or by sending them a photo.
Q: What is the best soap for breast cancer patients?
Ans - Gentle, fragrance-free soaps are best to avoid irritation and dryness. Look for options labeled for sensitive skin.
Disclaimer: All content and information provided in connection with Manta Cares is solely intended for informational and educational purposes only. This content and information is not intended to be a substitute for medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.