Introduction
Maintaining oral health is crucial for everyone, but it becomes even more vital for patients undergoing cancer treatments such as tamoxifen, chemotherapy, and bone health drugs. These treatments can significantly impact oral health, potentially leading to a range of dental issues. Manta Cares was founded by breast cancer survivors and we want to use our experience to help breast cancer patients and their family members navigate a life-altering diagnosis and continue to maintain a healthy lifestyle. Understanding the side effects of cancer drugs and how to manage them is key to ensuring a better quality of life during and after treatment. This article aims to shed light on the dental side effects of these cancer therapies and provide practical tips for maintaining oral health.
Overview of Cancer Treatments and Oral Health
Tamoxifen, chemotherapy, and bone health drugs are common treatments used for cancer, particularly breast cancer. Tamoxifen is a type of hormone therapy primarily used to treat hormone receptor-positive breast cancer. It works by blocking estrogen receptors on cancer cells which slows or halts the growth of tumors that depend on estrogen to thrive. While tamoxifen is a crucial part of treatment for many patients, it may lead to dry mouth and gum issues due to hormonal changes affecting oral tissues.
Chemotherapy involves the use of powerful drugs designed to kill rapidly dividing cancer cells. These drugs are effective at targeting cancer but can also affect normal, healthy cells, including those in the mouth. Chemotherapy can cause a broad spectrum of oral problems, including sores, sensitivity, and a heightened risk of infections due to its impact on the mucous membranes and salivary glands.
Bone health drugs, such as the bisphosphonates (zoledronate and others) and monoclonal antibodies (denosumab, romosozumab,and others) are medications used to treat or prevent bone complications, and are commonly prescribed to patients with cancer that has spread to the bone or those at high risk of bone issues such as osteoporosis. These drugs work by increasing bone density, preventing bone loss and strengthening bones. However, bone health drugs can lead to more severe complications like osteonecrosis of the jaw, which affects the bones in the mouth and can cause pain and tooth loss.
These treatments, while crucial, can have unintended effects on oral health. Let's delve into the specific dental side effects associated with each of these therapies.
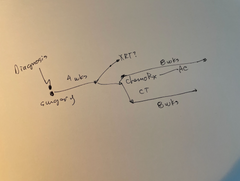
Cancer Maps to help you find your way, one decision at a time.Built for Patients, by Patients. Backed by World-Leading Oncologists

Dental Side Effects of Breast Cancer Treatment (Tamoxifen and Chemotherapy)
Tamoxifen and chemotherapy can both lead to gum issues. Patients might experience gum swelling, tenderness, or bleeding. This is due to the impact of these treatments on the mucous membranes and blood vessels in the mouth.
Chemotherapy often causes changes in the mouth that can lead to increased sensitivity in the teeth. This can be particularly uncomfortable when consuming hot, cold, or acidic foods and beverages.
One of the most common and painful side effects of chemotherapy is the development of mouth sores or ulcers. These sores can make eating, drinking, and even speaking uncomfortable.
Tamoxifen, chemotherapy, and bone drugs can all contribute to dry mouth, or xerostomia. This condition arises when the salivary glands are not producing enough saliva, which can lead to difficulties in speaking, swallowing, and a higher risk of oral infections.
The combination of a compromised immune system from chemotherapy and changes in oral health can make patients more susceptible to infections in the mouth. These infections can range from fungal infections like thrush to bacterial infections.
Long-term use of bone health drugs can lead to a condition known as osteonecrosis of the jaw (ONJ). This serious condition can result in tooth loss due to the deterioration of bone tissue in the jaw.
Bone drugs can also cause jaw pain and discomfort, which may be related to ONJ or other bone-related side effects. This can interfere with normal chewing and speaking functions. Studies have found that there is an increased risk for Bisphosphonate Related Osteonecrosis of the Jaw (BRONJ) in patients who receive bisphosphonate intravenously than those who receive the drug orally.
Preventing Dental Side Effects
Maintaining good oral hygiene is essential for preventing and managing the dental side effects of cancer treatments. Here are some tips to help:
- Brushing Your Teeth Twice a Day: Use a soft-bristled toothbrush to avoid irritating your gums and enamel.
- Brushing Your Tongue: This helps remove bacteria and can reduce bad breath.
- Using a Mild-Flavored Toothpaste with Fluoride: Opt for toothpaste that is gentle and fluoride-rich to help protect your teeth.
- Flossing Once Every Day: Flossing helps remove food particles and plaque from between your teeth and under the gumline.
- Avoiding Smoking and Vaping: Tobacco and vaping products can exacerbate oral health issues and should be avoided. There is evidence that smoking during cancer treatment can negatively influence the benefits from the treatment.
We always recommend keeping track of side effects you are experiencing so you can share that with your doctor. Check out the Manta Planner, which helps you track symptoms, stay organized and take notes during appointments.
Tell your dentists if you have recently received a bone health drug.
Your dentist may modify your dental treatment plan based on your exposures to these drugs.
Resources and Support for Breast Cancer Survivors
The Manta Cares team is composed of cancer survivors, caregivers and oncologists - so we truly understand the challenges that come with a cancer diagnosis because we’ve been there. We are here to walk with you as you go through your own cancer experience. Please don’t hesitate to reach out with any questions. Be sure to subscribe to our newsletter and check out our free resources like our Chemotherapy Checklist for Caregivers, Financial Checklist for Cancer Treatment and more. We also put out a bi-weekly podcast called the Patient from Hell to educate, empower and hopefully inspire you as you go through this crappy experience. You can listen on Spotify, Apple Podcasts, YouTube or anywhere you listen to podcasts. Dealing with cancer as a patient or caregiver can feel really lonely. Just know that you are not alone in this experience.
Related Articles:
- Tamoxifen Withdrawal Symptoms
- Does Tamoxifen Stop Periods?
- Does Tamoxifen Cause Acne?
- Heavy Period after Stopping Tamoxifen
- Weight Gain while on Tamoxifen
- Taxol 12 Weekly Treatments Side Effects
- Why Do Aromatase Inhibitors Cause Insomnia?
Conclusion
Studies and anecdotal evidence show that patients undergoing treatments like tamoxifen, chemotherapy, and bone drugs are at increased risk of experiencing oral side effects. According to a 2015 study, dental hygienists found increased gum related complications in patients using anti-estrogen therapies. Being proactive about dental care and seeking support can help manage these challenges and improve overall well-being. Remember, maintaining good oral hygiene and accessing available resources are key steps in ensuring that your oral health remains in good shape throughout your cancer experience.
Take charge with free, expert-crafted resources from Manta Cares—designed to support and empower cancer patients and their caregivers every step of the way. Explore now!
-
FREE Chemotherapy Checklist for Caregivers
- FREE Quick Start Guide to a Cancer Diagnosis
- FREE Gift-Giving Guide
- FREE Caregiver Communication Guide
- Life Wheel Audit: A simple exercise to re-center, re-prioritize and re-start new habits
- Eating the rainbow. Free shopping guide
- Free Financial Checklist for Cancer Treatment
- FREE Reflection Exercise
FAQs on Dental Side Effects Of Tamoxifen, Chemo and Bone Drugs
Q: Does Tamoxifen Cause Dental Problems?
Ans - Tamoxifen itself is not commonly associated with significant dental problems. However, it can cause dryness of the mouth, which may contribute to dental issues over time. Maintaining good oral hygiene and staying hydrated can help mitigate these effects. If you notice any persistent dental problems, consult your dentist for personalized advice.
Q: Does Chemotherapy Have Dental Side Effects?
Ans - Yes, chemotherapy can have several dental side effects. These may include mouth sores (stomatitis), dry mouth, changes in taste, and increased risk of infections. Chemotherapy can also lead to changes in the lining of the mouth, making it more susceptible to discomfort and complications.
Q: Does Tamoxifen Affect Bone Density?
Ans - Tamoxifen has a variable impact on bone density. It can actually have a protective effect on bone density in premenopausal women, but in postmenopausal women, it may not be as protective. Women taking tamoxifen, especially those who are postmenopausal, should have their bone health monitored regularly, as changes in bone density can increase the risk of osteoporosis.
Q: How Does Breast Cancer Affect Oral Health?
Ans - Breast cancer itself does not directly affect oral health, but the treatment can. For example, treatments like chemotherapy and radiation can lead to oral health issues such as dry mouth, mouth sores, and changes in taste. These side effects can impact overall oral health and comfort.
Q: How Does Cancer Treatment Affect Oral Health?
Ans - Cancer treatments, including chemotherapy, radiation therapy, and certain targeted therapies, can significantly impact oral health. Common effects include dry mouth, mouth sores, changes in taste, and increased risk of infections. Good oral hygiene and regular dental check-ups are crucial during and after treatment to manage these side effects.
Q: What Are the Oral Effects of Chemotherapy?
Ans - Chemotherapy can lead to several oral effects, such as:
- Mouth Sores: Painful sores or ulcers in the mouth.
- Dry Mouth: Reduced saliva production, leading to discomfort and a higher risk of cavities.
- Changes in Taste: Altered or diminished sense of taste.
- Gingivitis: Inflammation and bleeding of the gums.
- Increased Risk of Infections: Due to a weakened immune system.
Managing these effects involves maintaining excellent oral hygiene, staying hydrated, and using specific oral care products recommended by your dentist or healthcare provider.
Disclaimer: All content and information provided in connection with Manta Cares is solely intended for informational and educational purposes only. This content and information is not intended to be a substitute for medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.