Introduction
Chemotherapy often plays a crucial role in cancer treatment by using powerful medicines to fight cancer cells in the body. These drugs work by either killing the rapidly dividing cancer cells or slowing down their growth. Chemotherapy is designed to target cancer cells specifically, helping to shrink tumors, kill cancer cells in small tumor deposits outside of the breast, and stop the cancer from spreading to other parts of the body. However, normal fast growing cells in the body can also be damaged. Unintended damage to normal cells can lead to chemotherapy side effects, like hair loss, mouth sores and nausea. Cancer doctors customize chemotherapy treatments to suit each patient's needs and the type of cancer they have. For many cancers, chemotherapy is an essential tool.
Key Takeaways
- Chemotherapy is a type of cancer treatment that uses powerful medicines to stop or slow down the growth of cancer cells in the body.
- One type of chemotherapy treatment given to some patients is called TCHP
- TCHP is four chemotherapy drugs used together to fight the cancer cells.
Table of Contents
- What are the medications involved in TCHP chemo?
- What Is TCHP Chemo?
- Types of Chemotherapy Drugs in TCHP
- TCHP Chemo Regimen / Chemotherapy Regimen
- How is TCHP chemo administered?
- 8 TCHP Chemotherapy Side Effects
- Do symptoms become more severe as chemo progresses?
- Worst day after chemo treatment?
- What are the treatment options for TCHP chemo side effects?
- Questions for your doctor at the beginning and end of chemotherapy
- How long do side effects from chemo last?
- FAQs
What are the medications involved in TCHP chemo?
TCHP chemotherapy, an acronym for the combination of docetaxel (Taxotere ®), carboplatin, trastuzumab (Herceptin ®), and pertuzumab (Perjeta ®), is a treatment regimen primarily used for breast cancer patients with HER2-positive tumors. This multi-drug approach aims to target and inhibit the overexpression of the HER2 protein, which is a key driver for this type of breast cancer. The chemotherapy drugs docetaxel and carboplatin are typically administered during the first 12 or 18 weeks, and pertuzumab for a year. While TCHP has helped improve outcomes for people, it is not without side effects. Common reactions to the docetaxel and carboplatin chemotherapy include nausea, fatigue, hair loss, and decreased blood cell counts. Rarely, cardiac toxicity is a concern due to the inclusion of trastuzumab and pertuzumab, both of which may impact the heart function. The severity and timing of side effects can vary among individuals, but typically, patients may experience more challenging side effects during the chemotherapy treatment course, with peak symptoms often occurring shortly after drug administration. Careful monitoring and supportive care are essential components of managing these side effects and ensuring the best possible therapeutic outcomes for patients undergoing TCHP chemotherapy.
What Is TCHP Chemo?
TCHP chemotherapy is a specialized treatment primarily used for people diagnosed with breast cancer, specifically those with HER2-positive tumors. This therapeutic approach combines four different medications: docetaxel, carboplatin, trastuzumab, and pertuzumab. The main goal is to target and stop the overexpression of the HER2 protein, a crucial factor in the aggressive growth of certain types of breast cancer. By utilizing this multi-drug regimen, oncologists aim to disrupt the mechanisms that fuel the cancer's progression. TCHP has demonstrated effectiveness in improving outcomes for patients with HER2-positive breast cancer, with this 2022 study reporting a 3-year event-free survival of 90% in real world experience. This treatment plays a significant role in the comprehensive care strategy for those facing this particular form of breast cancer.
Types of Chemotherapy Drugs in TCHP
There are four types of drugs used in the TCHP chemotherapy regimen. Those drugs are:
- Docetaxel: Docetaxel is a chemotherapy drug that interferes with the growth and spread of cancer cells by disrupting their ability to divide and multiply.
- Carboplatin: Carboplatin is a platinum-based chemotherapy medication that works by damaging the DNA inside cancer cells, preventing them from growing and dividing.
- Trastuzumab: Trastuzumab is a targeted therapy drug that specifically targets cancer cells with an excess of HER2 protein, blocking a growth signal, inhibiting their growth and promoting immune system attacks against them.
- Pertuzumab: Pertuzumab is another targeted therapy that, in combination with trastuzumab, works to block HER2 protein signals, hindering the growth of HER2-positive breast cancer cells.
These drugs, when combined in the TCHP chemotherapy regimen, create a powerful treatment strategy to combat HER2-positive breast cancer by targeting various aspects of cancer cell growth and division. (Unrelated, but a recent cancer survivor and guest on our Patient from Hell podcast commented about how chemotherapy drug names sound suspiciously like they could be Star Wars villain names… I couldn’t help but agree – food for thought!)
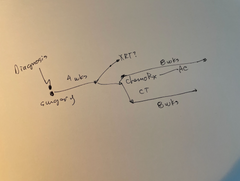
TCHP Chemo Regimen / Chemotherapy Regimen
TCHP chemotherapy drugs are typically administered in a specific schedule based on the treatment plan designed by oncologists. The timing and frequency of TCHP administration depend on factors such as the stage of the cancer, the patient's overall health, and the individualized treatment approach. Generally, TCHP is given in cycles, with each cycle lasting several weeks.
How is TCHP chemo administered?
The drugs are often administered intravenously, meaning they are delivered directly into the bloodstream through a vein. This method allows for efficient distribution of the medications throughout the body, targeting cancer cells wherever they may be present. The choice of intravenous administration ensures a controlled and precise delivery of the drugs, optimizing their effectiveness against HER2-positive breast cancer. The treatment schedule and mode of administration are crucial elements in tailoring TCHP chemotherapy to each patient's unique circumstances, aiming to achieve the best possible therapeutic outcomes.
8 TCHP Chemotherapy Side Effects
While TCHP is helpful in treating breast cancer, it does tend to cause other side effects. As a patient, that was one of the most disheartening parts of chemo for me – the drugs that would help fight my cancer were also going to make me feel sick. Some of the more common side effects seen with TCHP chemo are:
- Nausea and Vomiting: TCHP chemotherapy can lead to nausea and vomiting, which may vary in severity. Anti-nausea medications are often prescribed to manage these side effects.
- Fatigue: Patients undergoing TCHP chemotherapy may experience fatigue, a persistent feeling of tiredness or weakness. Adequate rest and regular physical activity within individual limits can help alleviate this symptom.
- Hair Loss: A common side effect of chemotherapy, TCHP can lead to partial or complete hair loss. This is usually temporary, and hair typically begins to grow back after the completion of the chemotherapy portion of the treatment.
- Decreased Blood Cell Counts: TCHP may impact blood cell production, leading to lowered levels of red blood cells (anemia), white blood cells (neutropenia), and platelets (thrombocytopenia). This can result in increased susceptibility to infections, fatigue, and easy bruising or bleeding.
- Cardiac Toxicity: Due to the inclusion of trastuzumab and pertuzumab, TCHP chemotherapy may pose a risk of cardiac toxicity, affecting the heart's function. Regular cardiac monitoring is crucial during treatment to detect and mitigate potential heart-related issues.
- Diarrhea: Some patients may experience diarrhea as a side effect of TCHP chemotherapy. It is essential to stay hydrated and notify healthcare providers if diarrhea becomes severe or persistent.
- Allergic Reactions: Allergic reactions to any of the drugs in TCHP are possible, although rare. Symptoms may include rash, itching, swelling, or difficulty breathing. Immediate medical attention is necessary if allergic reactions occur.
- Changes in Taste or Appetite: TCHP chemotherapy can alter taste perception and appetite. Maintaining a balanced diet and trying different foods may help manage these changes.
It's important to note that the severity and occurrence of these side effects can vary among individuals, and healthcare providers work closely with patients to monitor and address any challenges during the course of TCHP chemotherapy. Sometimes it is helpful to keep track of side effects on an ongoing basis. The Manta Planner helps organize symptom reporting, medication management and reminds you to keep notes to mention at doctor appointments.
In a 2022 study of 447 patients on a TCHP chemo regimen, the top reported side effects were:
- Anemia (89.9%) was the most commonly observed adverse event followed by thrombocytopenia (29.8%)
- Mucositis (85.2%), Pain (83.2%), and diarrhea (70.5%) were the most common non-hematologic adverse events
Do symptoms become more severe as chemo progresses?
The severity of symptoms during TCHP chemotherapy can vary from person to person, and the progression of symptoms may not necessarily follow a uniform pattern. However, it is common for certain side effects to become more pronounced during the course of treatment.
Immediate (onset hours to days) & Early (onset days to weeks)
Typically, patients may experience heightened symptoms shortly after the administration of the chemotherapy drugs, reaching a peak in the days following each session. This pattern may contribute to an accumulation of side effects over successive treatment cycles. For instance, nausea, fatigue, and decreased blood cell counts may become more noticeable as the chemotherapy progresses.
Late (onset weeks to months)
Additionally, factors such as the cumulative impact on the body and individual variations in tolerance levels can influence the overall intensity of symptoms. Despite the potential for increased severity, healthcare providers actively monitor patients, adjust treatment plans as needed, and provide supportive care to manage and alleviate the side effects, ensuring the best possible quality of life throughout the TCHP chemotherapy regimen.
Delayed (onset months to years)
While TCHP chemotherapy primarily aims to address the immediate challenges associated with breast cancer treatment, some patients may experience long-term side effects. It's important to note that the occurrence and severity of these effects can vary among individuals. Long-term side effects of TCHP chemotherapy may include:
- Cardiac Issues: The drugs trastuzumab and pertuzumab, components of TCHP, may pose a risk of long-term cardiac toxicity, potentially impacting heart function. Ongoing cardiac monitoring is crucial for detecting and managing any cardiac-related complications.
- Cognitive Impairment: Some individuals undergoing chemotherapy may report long-term cognitive changes, commonly referred to as "chemo brain." This can manifest as difficulties with memory, concentration, and mental clarity.
- Infertility: Chemotherapy, including TCHP, can affect fertility in both men and women. Long-term reproductive implications may include difficulty conceiving or an increased risk of early menopause.
- Peripheral Neuropathy: Long-term nerve damage, known as peripheral neuropathy, is a potential side effect of TCHP chemotherapy. This can result in tingling, numbness, or pain in the hands and feet.
- Bone Health: Chemotherapy may impact bone health, leading to long-term issues such as osteoporosis or an increased risk of fractures.
- Secondary Cancers: Some chemotherapy agents, although effective against the primary cancer, may increase the risk of developing secondary cancers over the long term. The components of TCHP, in the doses and schedule used, are not high risk for development of secondary cancers. Regular cancer screenings are essential for early detection and management.
It's crucial for patients to discuss potential long-term side effects with their healthcare team, and ongoing follow-up care is important to monitor and address any lasting effects of TCHP chemotherapy. Additionally, supportive measures and lifestyle adjustments may be recommended to manage these long-term consequences and promote overall well-being.
Worst day after chemo treatment?
Every person is different in their reaction to TCHP chemo, but our community has reported that the worst days after a chemotherapy infusion tend to be days 3-5.This often coincides with the stopping of the corticosteroids (typically decadron) used to prevent docetaxel side effects. Many find it helpful to taper the decadron over two or three days, rather than stopping abruptly. Talk with your oncologist about this. Most people report a cumulative effect, with later infusions hitting them harder than the first couple of rounds of chemo. Some people have reported that fatigue tends to hit first followed by nausea and exhaustion. At the peak of my chemo treatments, I remember getting winded walking from the couch about 20 yards to my kitchen. Remember, every person is different, so your experience might be completely different from someone else’s. I found that it was helpful to assume that I would need more help with household chores and caring for my kids as my chemo went along. I’ve never been good at asking for help, but the support from my family and friends during that time was invaluable. It was worth it to ask and people were really happy to have some tangible way they could help me and my family.
What are the treatment options for TCHP chemo side effects?
There are often medications or support services, known as palliative care, that can help manage the side effects of the chemotherapy drugs. Some of those include:
- Anti-Nausea Medications: To manage nausea and vomiting associated with TCHP chemotherapy, healthcare providers often prescribe anti-nausea medications. These medications can help alleviate or prevent these symptoms.
- Pain Medications: Patients experiencing pain, whether from chemotherapy-induced neuropathy or other side effects, may be prescribed pain medications to improve their comfort and quality of life.
- Cardiac Monitoring and Interventions: Regular monitoring of cardiac function is crucial for patients on TCHP chemotherapy. Depending on the findings, interventions such as adjusting the chemotherapy dosage or incorporating cardiac medications may be necessary.
- Supportive Care for Decreased Blood Cell Counts: Patients with lowered blood cell counts may receive supportive care, including blood transfusions or medications to stimulate blood cell production, to prevent complications such as infections or anemia.
- Counseling and Cognitive Support: For those experiencing cognitive changes or "chemo brain," counseling and cognitive rehabilitation may be beneficial. These services can provide strategies to cope with memory and concentration issues.
- Physical Therapy: Physical therapy can be helpful for managing peripheral neuropathy and maintaining mobility. Exercises and interventions provided by a physical therapist can address specific issues related to nerve damage.
- Bone Health Interventions: Patients at risk of bone health issues may receive supplements such as calcium and vitamin D or medications to support bone density. Weight-bearing exercises can also contribute to bone health.
- Psychosocial Support: Coping with the emotional and psychological aspects of cancer treatment is crucial. Psychosocial support, such as counseling or support groups, can help patients navigate the challenges associated with TCHP chemotherapy.
- Regular Cancer Screenings: Due to the potential risk of secondary cancers, ongoing surveillance through regular screenings for various cancers is essential for early detection and intervention.
It's important for anyone undergoing TCHP chemotherapy to communicate openly with your healthcare team about any side effects you are experiencing, as timely interventions and adjustments to the treatment plan can significantly improve your overall treatment experience. You do not need to suffer in silence! If you need a place to take notes before and during appointments to stay organized, take a look at the Manta Notebook.
Questions for your doctor at the beginning and end of chemotherapy
When I was diagnosed with cancer, I remember feeling like I was “dropped into Cancerland”, and that I “didn’t know what I didn’t know”. I found it helpful to prepare questions for my doctor before my appointments so that I felt more prepared. Here are some questions to consider asking your doctor before you start chemo.
Before TCHP Chemotherapy:
Treatment Plan Clarification:
- What is the overall treatment plan, and how long is the expected duration of TCHP chemotherapy?
Side Effects and Expectations:
- What are the common side effects associated with TCHP, and how can they be managed?
- What side effects should I report immediately, and which ones are considered more typical?
Cardiac Monitoring:
- How will my heart be monitored during and after TCHP chemotherapy?
- What measures are in place to address any potential cardiac issues?
Fertility Considerations:
- Are there potential impacts on fertility, and should I consider fertility preservation options before starting treatment?
Supportive Care:
- Are there supportive care measures or medications available to alleviate side effects such as nausea, pain, or fatigue?
Alternative Treatment Options:
- Are there alternative or complementary therapies that may be beneficial in conjunction with TCHP chemotherapy?
After TCHP Chemotherapy:
And here are a few questions to consider asking as you are finishing up your chemotherapy treatment. Again, I found it helpful to write these out before my appointments because I tended to feel emotionally overwhelmed while I was sitting with my doctor, and would end up forgetting everything I had meant to ask. (The Manta Planner is a useful tool to help with this!). Here are some questions you might consider asking:
Effectiveness Assessment:
- How will we assess the effectiveness of TCHP chemotherapy in treating my cancer?
- What follow-up tests or imaging will be performed to monitor my progress?
Long-Term Side Effects:
- What potential long-term side effects should I be aware of, and how will they be managed?
- Are there any specific symptoms that warrant immediate attention post-treatment?
Cardiac Health Follow-Up:
- Will there be ongoing monitoring of my cardiac health, and what steps will be taken if any issues arise?
Recovery Timeline:
- What is the expected recovery timeline after completing TCHP chemotherapy?
- When can I expect a return to normal activities and routine screenings?
Follow-Up Care Plan:
- What is the recommended schedule for follow-up appointments and cancer screenings?
- Are there any specific signs or symptoms I should watch for between appointments?
Psychosocial Support:
- Are there resources or recommendations for psychosocial support during the post-treatment phase?
- How can I address any lingering emotional or psychological effects of TCHP chemotherapy?
Asking these questions can help ensure that you have a clear understanding of your treatment plan, potential side effects, and post-treatment care, facilitating effective communication with your healthcare team.
Cancer Maps to help you find your way, one decision at a time.Built for Patients, by Patients. Backed by World-Leading Oncologists

How long do side effects from chemo last?
The duration of side effects from TCHP chemotherapy can vary widely among individuals, and the persistence of these effects is influenced by several factors. Common side effects, such as nausea, fatigue, and hair loss, are often temporary and may begin to improve shortly after completing the TCHP regimen. However, some individuals may experience lingering or late-emerging effects, particularly related to long-term issues like cardiac health, fertility, and peripheral neuropathy. Cardiac effects may persist, necessitating ongoing monitoring, and peripheral neuropathy might endure for an extended period after treatment completion. Hair loss is usually reversible, with hair starting to grow back after the chemotherapy concludes. It's essential for individuals to discuss their specific situation with their healthcare team, as they can provide personalized insights into the expected duration of side effects and strategies to manage or mitigate any lingering challenges. Regular follow-up appointments and open communication with healthcare providers contribute to a comprehensive understanding of the post-treatment phase and help address any ongoing concerns.
Read more:
- How To Lose Weight On Letrozole?
- Can Claritin Help With Joint Pain From Breast Cancer Treatment?
- Side Effects of AC followed by Taxol Chemo
- Taxol 12 Weekly Treatments Side Effects
- Tamoxifen Withdrawal Symptoms
FAQs on TCHP Chemotherapy: Which Days are the Worst?
Q: How long does it take to recover from TCHP chemo?
Ans - Recovery from TCHP chemo varies for each person, but it often takes a few weeks to feel better after finishing the treatment. Some side effects may go away quickly, while others might last longer, and the healthcare team will help you understand what to expect during the recovery process.
Q: How many rounds of TCHP are there?
Ans - The number of TCHP chemo rounds depends on the individual's cancer and treatment plan, but usually, people have several rounds over a few months. The healthcare team will discuss the specific number of rounds and the schedule based on your unique situation.
Q: What to expect during TCHP chemo?
Ans - During TCHP chemotherapy treatments, you'll likely go to the hospital or clinic regularly to receive medicine through a vein in your arm. The actual treatment can take several hours. You might feel tired, nauseous, or lose your hair during this time, but your healthcare team will help manage these side effects. They'll also monitor your heart and overall health to make sure you're doing okay throughout the process.
Q: Will I lose my hair with TCHP?
Ans - Yes, some people may lose their hair during TCHP chemotherapy. It's a common side effect, but your healthcare team can provide support and discuss options, such as wigs or scarves, to help you feel more comfortable during this time.
Q: Does TCHP chemo cause weight gain?
Ans - TCHP chemotherapy might lead to changes in weight, but it doesn't always cause weight gain. Some people may experience weight loss due to nausea or changes in appetite during treatment. It's important to talk to your healthcare team about any concerns you have regarding weight changes, and they can provide guidance and support to help you maintain a healthy and comfortable weight during TCHP chemotherapy.
Q: How long does TCHP treatment last?
Ans - TCHP treatment usually lasts about 6 months. You'll get medicine every 3 weeks, for a total of 6 times. This varies by individual, however, so be sure to ask your doctor about what to expect for your specific situation.
Q: Can you exercise during breast cancer treatment?
Ans - Yes, you can exercise during breast cancer treatment. Light exercise like walking can help you feel better, but talk to your doctor about what's safe for you. Check out this list of exercises cancer patient Mike Linn put together (and check with your doctor before you start a fitness program!).
Q: Should I take my nausea medications when I’m not nauseous?
Ans - It's best to take your nausea medicine on schedule, even if you don't feel sick. This helps prevent nausea before it starts. But make sure you consult with your doctor about what’s right for your specific situation.
Q: How often is monitoring needed?
Ans - Your doctor will check on you before each treatment, about every 3 weeks. They might do more checks if you have side effects.
Disclaimer: The content provided by Manta Cares Inc. is intended for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website.
While we strive to keep the information up to date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the website or the information, products, services, or related graphics contained on the website for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
The use of our platform does not create a doctor-patient relationship. Manta Cares Inc. does not recommend or endorse any specific tests, physicians, procedures, opinions, or other information that may be mentioned on the site. Reliance on any information provided by Manta Cares Inc., Manta Cares Inc. employees, others appearing on the site at the invitation of Manta Cares Inc., or other visitors to the site is solely at your own risk.
The site may contain health- or medical-related materials that are sexually explicit. If you find these materials offensive, you may not want to use our site. The site and the content are provided on an "as is" basis.