Introduction
As you deal with breast cancer, you might be using or considering aromatase inhibitors (AIs), drugs that lower your estrogen levels, as a treatment. Studies have found that AIs have many benefits, such as reducing the risk of recurrence and improving survival rates of breast cancer in some patients. Before deciding to use AIs for your cancer, you should know what side effects to expect. The immediate side effects can include hot flashes, joint and muscle pain, hair thinning, and insomnia. A long term side effect may be bone thinning or osteoporosis.
All of us at Manta Cares understand how difficult it is to navigate all the complex decisions you face in your diagnosis. Our goal is to help make your experience a little easier by providing guidance and making sure you have all the necessary information to make informed decisions on your treatment at your disposal. In this article, we will explore one of the most common AI side effects: insomnia.
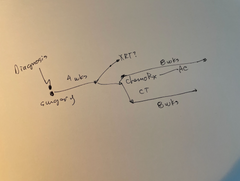
*** Feeling lost after a cancer diagnosis? We are launching digital maps this Fall to show you the paths you might face during your experience as well as provide you with education and resources at each map “station” along the way. Join the Manta Maps access list here. ***
What are Aromatase Inhibitors?
Aromatase inhibitors (AIs) are a class of medications used primarily in the treatment of hormone receptor-positive breast cancer, which depends on estrogen signaling to grow. These drugs work by blocking the enzyme aromatase, which is responsible for converting androgens (produced by the adrenal glands and fat tissues) into estrogens (particularly estradiol) in postmenopausal women. By inhibiting aromatase, AIs reduce the levels of estrogen circulating in the body, thus depriving hormone-sensitive breast cancer cells of the hormone they need to grow and multiply.
Aromatase inhibitors are typically used as adjuvant therapy, neoadjuvant therapy, or first-line therapies in metastatic breast cancer. Adjuvant therapy is administered after primary treatments (surgery or radiation therapy) to reduce the risk of breast cancer recurrence. In a study conducted on the efficacy of long term adjuvant therapy using the AI letrozole, it was found that women who received letrozole had a 95% rate of 5-year disease-free survival compared to 91% in the control group. Neoadjuvant AI therapy is administered before surgery and used to facilitate surgery by making tumors smaller and easier to remove. Metastatic breast cancer is when the cancer has spread across the body and therefore is difficult to surgically remove. In this case, AI can be used as a primary treatment to prevent further dispersion of breast cancer throughout the body. AIs are particularly effective in postmenopausal women because their ovaries no longer produce significant amounts of estrogen, and most of their estrogen comes from peripheral conversion of androgens in tissues like fat.
There are currently three aromatase inhibitors in use in the US. They are all oral pills and work similarly. Common FDA approved AI medications include Anastrozole (brand name: Arimidex), Letrozole (brand name: Femara), and Exemestane (brand name: Aromasin). Though the three have never been compared one against the other, most oncologists consider them to have equal anti cancer benefit. The side effects differ among the three. While they are all AIs, each of these drugs have slightly differing properties. Anastrozole and Letrozole are non-steroidal aromatase inhibitors, whereas Exemestane is a steroidal aromatase inhibitor. Anastrozole and Letrozole are often used as first-line treatments for postmenopausal women with hormone receptor-positive breast cancer. Exemestane may be used as an alternative or in cases where other aromatase inhibitors are not tolerated. Anastrozole and Letrozole are metabolized primarily in the liver, whereas Exemestane is metabolized in the liver and other tissues.
The aromatase inhibitors and tamoxifen are often used to treat estrogen receptor positive breast cancer. For information on tamoxifen see: Side Effects Of Tamoxifen
Link Between Aromatase Inhibitors and Insomnia
The disruption in hormone levels caused by AIs can have adverse effects on one’s sleep cycle, as estrogen regulates the sleep-wake cycle, sometimes leading to insomnia. Reducing estrogen levels makes it more difficult for patients to fall asleep or stay asleep throughout the night. AIs can also lead to insomnia in other ways. AIs can induce symptoms similar to those experienced during menopause, such as hot flashes and night sweats which disrupt sleep patterns.
Detailed Look at How Aromatase Inhibitors Cause Insomnia
AIs can cause insomnia because of both biological mechanisms and psychological impacts of being diagnosed with cancer.
Biologically, insomnia is a side effect of AIs because of the impact of estrogen suppression on one’s sleep cycle.
Estrogen plays a role in regulating neurotransmitters in the brain, including serotonin, dopamine, and norepinephrine, which are involved in sleep-wake cycles and mood regulation. Reduced estrogen levels due to AI treatment can lead to changes in these neurotransmitter systems. For instance, serotonin is important for promoting sleep and a sense of well-being, and alterations in its levels can affect sleep quality. Disruption in these neurotransmitter systems can contribute to difficulty falling asleep (sleep onset insomnia), staying asleep (sleep maintenance insomnia), or both.
Estrogen also plays a role in regulating the body's circadian rhythm, which is the internal process that regulates the sleep-wake cycle which is usually over a 24-hour period. Circadian rhythm is influenced by the secretion of hormones like melatonin, which promotes sleepiness, and cortisol, which helps regulate wakefulness. Changes in estrogen levels can disrupt this delicate balance, leading to disturbances in the timing and quality of sleep.
Estrogen receptors are present in various regions of the brain that regulate sleep, including the hypothalamus and brainstem. Estrogen receptors in these areas can directly influence neuronal activity related to sleep patterns and sleep quality. Reduction in estrogen levels through AI treatment may alter the activity of these sleep regulatory centers, potentially leading to insomnia.
Rapid eye movement (REM) sleep is a stage of sleep associated with dreaming and important for cognitive function and emotional processing. Estrogen influences the duration and quality of REM sleep. Reduction in estrogen levels can disrupt REM sleep patterns, leading to less restorative sleep and contributing to overall sleep disturbances.
In addition to the biological mechanisms, the psychological impact of aromatase inhibitors (AIs) on insomnia is significant, especially in the context of cancer treatment. Here’s how AIs can contribute to insomnia through psychological pathways:
Stress and Anxiety:
A breast cancer diagnosis and subsequent treatment with AIs can cause significant psychological distress. Patients often experience fear, worry about treatment outcomes, and uncertainty about the future. This stress and anxiety can disrupt normal sleep patterns. Heightened stress levels activate the body’s sympathetic nervous system, leading to increased alertness and difficulty relaxing, which are counterproductive to falling asleep and maintaining sleep throughout the night. Patients may develop anticipatory insomnia, where they worry excessively about not being able to sleep even before bedtime, which can exacerbate actual sleep difficulties.
Depression and Mood Changes:
Cancer treatment, including hormonal therapies like AIs, can sometimes lead to mood changes and depression. These mood alterations can contribute to insomnia by affecting sleep-wake cycles and making it harder to achieve restful sleep. Persistent sadness, loss of interest in activities, and feelings of hopelessness can disrupt the ability to relax and fall asleep.
Coping Mechanisms:
Some patients may develop maladaptive coping behaviors in response to the stress of cancer treatment, such as excessive use of caffeine or alcohol, which can interfere with sleep patterns. Disrupted daily routines and irregular sleep schedules can contribute to insomnia. Patients may find it difficult to maintain a consistent sleep-wake cycle due to treatment-related appointments, medication schedules, and emotional upheaval.
Impact of Treatment Side Effects:
Side effects of AIs, such as joint pain or hot flashes, can contribute to physical discomfort that disrupts sleep. Pain and discomfort can make it difficult to find a comfortable sleeping position or to stay asleep throughout the night. Some patients may experience side effects from medications prescribed alongside AIs, such as corticosteroids or anti-nausea drugs, which can affect sleep patterns.
Addressing Insomnia: Practical Tips
Insomnia is treatable and can be addressed by making lifestyle changes and, if necessary, seeking medical help.
According to the NIH, some lifestyle changes one can make to deal with insomnia include keeping a regular sleep schedule, getting regular physical activity, and avoiding caffeine and, nicotine in the afternoon and evening, and avoiding alcohol, and recreational drugs. Also, avoid drinking large amounts of fluid before bedtime. Insomnia patients can also benefit from seeking medical intervention. This includes Cognitive Behavioral Therapy (CBT). In CBT, patients learn strategies such as stimulus control, relaxation methods, sleep restrictions, and light therapy, that can help reduce insomnia. Some people find use of a “white noise generator” and sleep blindfolds to be helpful.
Prescription medicines for insomnia include Doxepin hydrochloride (Silenor), Eszopiclone (Lunesta), Suvorexant (Belsomra), Temazepam (Restoril), and Zolpidem tartrate (Ambien, Ambien CR, Edluar). Some alternative treatments that patients can obtain without a prescription include melatonin, valerian, acupuncture, yoga, and meditation.
Cancer Maps to help you find your way, one decision at a time.Built for Patients, by Patients. Backed by World-Leading Oncologists

Related Articles:
- Tamoxifen Withdrawal Symptoms
- Letrozole and Weight Gain
- Taxol 12 Weekly Treatments Side Effects
- Side Effects of AC followed by Taxol Chemotherapy
- Can Claritin Help With Joint Pain From Breast Cancer Treatment?
Our team “gets it”
The Manta Cares team is composed of cancer survivors, caregivers and oncologists - so we truly understand the challenges that come with a cancer diagnosis because we’ve been there. We are here to walk with you as you go through your own cancer experience. Please don’t hesitate to reach out with any questions. Be sure to subscribe to our newsletter and check out our free resources like our Chemotherapy Checklist for Caregivers, Financial Checklist for Cancer Treatment and more. We also put out a bi-weekly podcast called the Patient from Hell to educate, empower and hopefully inspire you as you go through this crappy experience. You can listen on Spotify, Apple Podcasts, YouTube or anywhere you listen to podcasts. Dealing with cancer as a patient or caregiver can feel really lonely. Just know that you are not alone in this experience.
Conclusion
Addressing insomnia in breast cancer treatment is crucial for several reasons, highlighting its importance in improving overall quality of life and treatment outcomes. Insomnia significantly impacts a patient's quality of life by causing fatigue, irritability, and difficulty concentrating. Addressing sleep disturbances can enhance daily functioning and emotional well-being. Adequate sleep is essential for immune function, hormone regulation, and overall physical recovery. Managing insomnia can support the body's healing processes during cancer treatment. Sleep disturbances can exacerbate feelings of stress, anxiety, and depression, which are already heightened during cancer treatment. Improving sleep can positively influence mental health and resilience. Better sleep may improve adherence to treatment plans, including medications and therapies, which are critical for achieving optimal outcomes in breast cancer treatment. Effective management of insomnia demonstrates a commitment to comprehensive supportive care, addressing not only the cancer itself but also the side effects and challenges that impact a patient's well-being. Whether you are a survivor, caregiver, or a current cancer patient, Manta Cares is here to support you on your journey with cancer. Check out our website to learn more about the services and products we offer.
Take charge with free, expert-crafted resources from Manta Cares—designed to support and empower cancer patients and their caregivers every step of the way. Explore now!
-
FREE Chemotherapy Checklist for Caregivers
- FREE Quick Start Guide to a Cancer Diagnosis
- FREE Gift-Giving Guide
- FREE Caregiver Communication Guide
- Life Wheel Audit: A simple exercise to re-center, re-prioritize and re-start new habits
- Eating the rainbow. Free shopping guide
- Free Financial Checklist for Cancer Treatment
- FREE Reflection Exercise
FAQs - Why Do Aromatase Inhibitors Cause Insomnia?
Q: Can anastrozole cause insomnia?
Ans - Anastrozole, like other aromatase inhibitors, can potentially cause insomnia as a side effect. This is because these medications can disrupt hormone balance, which in turn may affect sleep patterns in some individuals.
Q: Why does letrozole cause insomnia?
Ans - Letrozole, another aromatase inhibitor, can cause insomnia due to its influence on hormone levels. Changes in estrogen levels, which letrozole effects, can impact sleep regulation mechanisms in the body.
Q: Why take anastrozole at night?
Ans - Taking anastrozole at night is sometimes recommended because it may help mitigate some of the potential side effects such as nausea or dizziness that can occur when taken during the day. However, the specific timing of medication should be discussed with a healthcare provider.
Q: Why are aromatase inhibitors bad for you?
Ans - Aromatase inhibitors are used primarily in breast cancer treatment to lower estrogen levels. While effective in treating hormone-sensitive cancers, they can have side effects such as joint pain, osteoporosis, and potential impact on cardiovascular health due to decreased estrogen levels.
Q: Does anastrozole cause sleeplessness?
Ans - Yes, anastrozole can cause sleeplessness or insomnia as a side effect. This is because it affects estrogen levels in the body, which can disrupt normal sleep patterns.
Q: Best time of day to take aromatase inhibitors?
Ans - The best time of day to take aromatase inhibitors can vary depending on individual factors and should be discussed with a healthcare provider. Taking them at night might help reduce certain side effects, but this varies among patients.
Q: Estrogen blocker insomnia?
Ans - Insomnia can be a side effect of medications that block estrogen, such as aromatase inhibitors (anastrozole, letrozole) and selective estrogen receptor modulators (tamoxifen). These medications affect hormone levels, which can disrupt sleep patterns.
Q: Tamoxifen insomnia treatment?
Ans - Treating insomnia caused by tamoxifen or similar medications may involve sleep hygiene practices (e.g., establishing a bedtime routine, avoiding caffeine before bed), behavioral therapies, or medications prescribed by a healthcare provider.
Q: Why do aromatase inhibitors cause joint pain?
Ans - Aromatase inhibitors can cause joint pain as a side effect because they lower estrogen levels in the body. Estrogen helps maintain bone density and joint health, so a decrease in estrogen can lead to joint stiffness and pain. Read more about joint pain here.
Disclaimer: The content provided by Manta Cares Inc. is intended for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website.
While we strive to keep the information up to date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the website or the information, products, services, or related graphics contained on the website for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
The use of our platform does not create a doctor-patient relationship. Manta Cares Inc. does not recommend or endorse any specific tests, physicians, procedures, opinions, or other information that may be mentioned on the site. Reliance on any information provided by Manta Cares Inc., Manta Cares Inc. employees, others appearing on the site at the invitation of Manta Cares Inc., or other visitors to the site is solely at your own risk.
The site may contain health- or medical-related materials that are sexually explicit. If you find these materials offensive, you may not want to use our site. The site and the content are provided on an "as is" basis.