Guest post by Mike Linn. Opinions are those of the author.
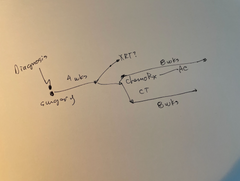
When I was first diagnosed with cancer in 2018, I assumed there would be some sort of system guiding my actions through every step of treatment. A doctor, nurse, or some… medical administrator sherpa would ensure I was whisked along step-by-step to give me the best care available for my physical health and long-term well-being.
This idea would soon be dashed by the reality of the American medical system.
Still, as a then-30-year-old with a then-girlfriend who worked in medicine, I next hoped that her expertise and network would provide easy solutions while I crumbled under the emotional toll of getting advanced melanoma seemingly out of nowhere.
Ultimately, I learned that while there are many kind people and well-intended resources available for cancer patients, the only way to access those and get the best care is to become an advocate for yourself - and quickly.
Here’s how to take your healthcare into your own hands.
Why Cancer Patients Need to Advocate For Themselves
I’ve long maintained that cancer patients should treat their cases like the most important job they’ve ever had. This is the literal definition of life or death.
Thus, self-advocacy during cancer treatment is critical for many reasons, including:
-
To any medical provider, scheduler, or facility, you are just part of their job. This isn’t an insult to them or a slight on their character, it’s just reality. Similarly, people make mistakes at their job no matter how competent they are. No one should care more or be more invested in your case than you in order to protect the progression of your care.
-
Most medical scheduling systems are inherently slow, and closed mouths don’t get fed. I have been able to expedite appointments by being willing to travel to hospitals in other cities, getting on waitlists, asking nicely, or even staging a sit-in at a medical imaging office.
-
The more proactive you are in your case, the more you will learn about the decisions being made in your care. Down the line, this will help you make better elective decisions about your health and other potential medical issues - especially if your cancer is aggressive, chronic, or recurrent.
- You have the most power as the patient in this situation. Caregivers, spouses, family members, and friends can and will help you, but in my experience “I’m a cancer patient” goes a long way in triggering someone to take action.
These are all compelling reasons, but it takes practice and effort to represent yourself well.
Examples of Self-Advocacy for Cancer Patients
It’s simple to say “Don’t take no for an answer” about medical needs, but this ignores many complications. Cancer treatment is stressful and often physically debilitating. Being your own advocate costs you time and money, and our bandwidth as cancer patients is typically less than normal.
I advise trying these things to advocate for yourself immediately:
Explore a second opinion proactively
This isn’t rude and doesn’t take too much time if done respectfully. Your doctor or medical team should be able to assist you with this, and it is reassuring to know that all the angles of your case are being seen.
Prioritize your needs
Cancer treatment is difficult and requires sacrifice. Try to keep your own sanity and preferences as priorities, even if that’s not your usual personality.
Take notes about your case
There will be lots of small specifics within your diagnosis that can help you or your medical team make better, quicker decisions. I advise taking notes in a journal or digital file that you can easily offer up to a doctor or office so that they have all the pertinent information.
(Our Manta Planner can help with this!)
Be willing to ask for help
It can be easy to feel like your case or situation is a burden to your loved ones or even medical professionals. This is not the case, and no one can navigate cancer alone. Find the people willing to be in your corner, even if it is an online advocacy group or friends you make on social media.
Your diagnosis and situation are unique, and self-advocacy is a skill. It might feel awkward to tell a doctor’s office that you’ll call back every morning to check on a waitlist the first time you do it. By day two of your cancer-care telethon, you’ll feel better about it. This isn’t the situation we asked to be in, but it’s up to us to approach it with zeal.
Dealing with cancer? Are you wondering “what’s next for me?”
The Manta Cares team is composed of cancer survivors, caregivers and oncologists - so we have asked that question ourselves. Which is why we created Your Cancer GPS™ to understand your options, the support available and what lies ahead in your cancer experience. We don’t have all the answers, but we can arm you with the questions to ask to ensure you’re getting the best possible care. Learn more here.
Be sure to subscribe to our newsletter and check out our free resources like our Chemotherapy Checklist for Caregivers, Financial Checklist for Cancer Treatment and more. We also put out a bi-weekly podcast called the Patient from Hell to educate, empower and hopefully inspire you as you go through this crappy experience. You can listen on Spotify, Apple Podcasts, YouTube or anywhere you listen to podcasts. Dealing with cancer as a patient or caregiver can feel really lonely. Just know that you are not alone in this experience.
About the author
Mike Linn is a writer, athlete, business owner, and now a cancer patient advocate. He was first diagnosed with stage 3c metastatic melanoma at the age of 30 and had a stage 4 recurrence in 2023 at 35. In a better effort to understand the mental health side of being a cancer patient, he began posting content to social media and support groups and has yet to stop talking about his cancer experience both personally and professionally. Mike also loves candy and is determined to dispel the notion that sugar specifically feeds cancer - or he is at least hopeful that research will prove this.
Disclaimer: All content and information provided in connection with Manta Cares is solely intended for informational and educational purposes only. This content and information is not intended to be a substitute for medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.