Author: Molly Lindquist
Medically reviewed by Dr. Doug Blayney on August 30, 2024.
Introduction
Cancer treatments have come a long way in recent years, offering hope and improved outcomes for many patients. However, as anyone who has undergone treatment knows, this journey often comes with challenges. While we often hear about common side effects like hair loss or nausea, there's a lesser-known but significant concern that deserves our attention: pulmonary toxicity. In this blog, we'll explore what pulmonary toxicity (another way of saying lung injury or damage) is, how it can arise from cancer treatments, and most importantly, what it means for you or your loved ones facing this challenge.
What is pulmonary toxicity?
Imagine your lungs as a delicate, intricate network of tissues – blood vessels, air sacs, tissues that separate the air from the blood, and tissues that hold it all together – that allow you to breathe easily and effortlessly. Pulmonary toxicity occurs when this network is damaged, leading to inflammation and scarring. It's as if the very air you breathe becomes a challenge, with your lungs struggling to perform their vital function.
This condition affects the entire respiratory system, from the airways to the tiny air sacs (alveoli) where oxygen exchange occurs. The result can be a range of breathing difficulties that impact your daily life and overall well-being.
What causes pulmonary toxicity?
While cancer treatments are designed to target cancer cells, sometimes they can affect healthy tissues too. Let's look at how different treatments can potentially lead to pulmonary toxicity.
Chemotherapy
Some chemotherapy drugs, while powerful allies in fighting cancer, can inadvertently damage lung tissues. Drugs like bleomycin, methotrexate, and cyclophosphamide are known to potentially cause lung issues. It's as if these medications, in their quest to eliminate cancer cells, sometimes mistake healthy lung cells for the enemy.
Radiation Therapy
When radiation is directed at tumors in the chest area, it can sometimes affect nearby lung tissue. This can lead to two main types of lung damage:
- Radiation pneumonitis: This is an early reaction, occurring within weeks or months of treatment. It's like an inflammatory response in your lungs, causing symptoms similar to pneumonia. Damage from radiation pneumonitis can be temporary if discovered and treated early.
- Radiation fibrosis: This is a late treatment effect, sometimes developing months or even years after treatment. It's characterized by scarring in the lungs, which can make breathing progressively more difficult over time.
Targeted Therapy and Immunotherapy
These newer treatments have revolutionized cancer care, but they too can have pulmonary side effects. For example, some targeted therapies can cause inflammation in the lungs. Immunotherapy, which boosts your immune system to fight cancer, can sometimes lead to your immune system mistakenly attacking healthy lung tissue.
Symptoms and Diagnosis:
Recognizing the signs of pulmonary toxicity is crucial. If you're undergoing cancer treatment and experience any of the following symptoms, it's important to discuss them with your healthcare team:
- A persistent, dry cough that doesn't seem to go away
- Shortness of breath, especially with activities that weren't previously challenging
- Chest pain or tightness
- Fatigue that seems out of proportion to your activity level
- Fever (in some cases)
These symptoms can be subtle at first, and it's easy to attribute them to the stress of cancer treatment or general fatigue. However, early detection is key to managing pulmonary toxicity effectively.
To diagnose pulmonary toxicity, your doctor may use a combination of tools:
- Physical examination and discussion of your symptoms
- Imaging tests like chest X-rays or CT scans to look for signs of inflammation or scarring in the lungs
- Pulmonary function tests to measure how well your lungs are working
- In some cases, a lung biopsy might be necessary to confirm the diagnosis
Management and Treatment Strategies
Facing pulmonary toxicity can be daunting, but there are ways to manage and even prevent it.
Preventive Measures:
- Before starting treatment, your healthcare team may perform baseline chest x-ray or lung function tests. This gives them a point of comparison to monitor any changes during treatment.
- Regular check-ups and open communication with your healthcare team are crucial. Don't hesitate to report any new symptoms, no matter how minor they might seem.
- If you smoke, quitting is one of the best things you can do to protect your lungs during treatment.
Treatment Options
- Corticosteroids are often the first line of defense against pulmonary toxicity. These medications help reduce inflammation in the lungs.
- Supportive care is crucial. This might include oxygen therapy to help with breathing, or pulmonary rehabilitation to improve lung function.
- Lifestyle adjustments can make a big difference. This might include gentle exercise to maintain lung capacity, breathing exercises, and avoiding respiratory irritants like air pollution or secondhand smoke.
Also Read: 12 Tips For Managing Side Effects From Breast Cancer Radiation
Impact on Quality of Life
Living with pulmonary toxicity can be challenging. Simple tasks like climbing stairs or carrying groceries might suddenly feel like monumental efforts. This physical limitation can be frustrating and may lead to feelings of anxiety or depression.
It's important to remember that these feelings are valid and normal. Many patients find that joining support groups or speaking with a therapist who specializes in working with cancer patients can be incredibly helpful. Remember, you're not alone in this journey.
Future Directions
The medical community is continuously working to improve cancer treatments while minimizing side effects like pulmonary toxicity. Researchers are exploring new ways to protect lung tissue during treatment, developing more targeted therapies that spare healthy cells, and investigating biomarkers that could predict which patients are at higher risk for developing pulmonary toxicity.
Our team “gets it”
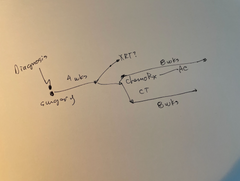
The Manta Cares team is composed of cancer survivors, caregivers and oncologists - so we truly understand the challenges that come with a cancer diagnosis because we’ve been there. We are here to walk with you as you go through your own cancer experience. Please don’t hesitate to reach out with any questions. We are even developing disease-specific step-by-step maps to show you all the paths you might face during your cancer experience and connect you with relevant support and resources. Sign up for access to our Manta Maps here.
Be sure to subscribe to our newsletter and check out our free resources like our Chemotherapy Checklist for Caregivers, Financial Checklist for Cancer Treatment and more. We also put out a bi-weekly podcast called the Patient from Hell to educate, empower and hopefully inspire you as you go through this crappy experience. You can listen on Spotify, Apple Podcasts, YouTube or anywhere you listen to podcasts. Dealing with cancer as a patient or caregiver can feel really lonely. Just know that you are not alone in this experience.
Related Articles:
- Cold Cap for Chemo
- How to Sleep with a Chemo Port
- How Your Body Might Change During Cancer Treatment
- Why Diet and Nutrition Are Important for Cancer Patients
Conclusion
Understanding and managing pulmonary toxicity is a crucial part of the cancer treatment journey. While it can be a challenging side effect, remember that knowledge is power. By being aware of the risks and symptoms, you can work proactively with your healthcare team to monitor your lung health and address any issues early.
If you're undergoing cancer treatment, don't hesitate to have open, honest conversations with your healthcare providers about your concerns. Ask about the potential risks of pulmonary toxicity with your specific treatment plan and what steps you can take to protect your lung health.
Remember, your well-being extends beyond just fighting the cancer – it's about maintaining the best possible quality of life throughout your treatment and beyond. By staying informed and proactive, you're taking an important step in advocating for your overall health and well-being.
References
- https://err.ersjournals.com/content/28/154/190012
- https://onlinelibrary.wiley.com/doi/full/10.1111/resp.13915
Disclaimer: All content and information provided in connection with Manta Cares is solely intended for informational and educational purposes only. This content and information is not intended to be a substitute for medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.