Author: Molly Lindquist
Guest post by Mike Linn. Opinions are those of the author. Medically reviewed by Dr. Doug Blayney on August 26, 2024.
When diagnosed with cancer, the first thing that you think is probably not, “Should I be jogging more?”
It’s more likely a string of internal expletives to express shock, terror, and sorrow, followed by trying to process a slew of information that goes in one ear and out the other.
By the time you get an individual diagnosis, prognosis, and treatment plan, you may have temporarily given up on your day-to-day habits while trying to navigate the alien-feeling world of being a cancer patient.
But don’t throw your jogging shoes in the closet too fast - working out might be a path to sanity and better treatment outcomes - and there’s evidence to back it up.
The Clinical Benefits of Exercise During Cancer Treatment
For decades, doctors have recommended exercise as part of a healthy lifestyle that helps prevent cancer. Similarly, there was anecdotal evidence that working out during treatment was generally good, but it wasn’t a clinical recommendation.
In 2024, there are sufficient studies to show that a workout routine is worth the time and energy if you are able to.
According to the American Cancer Society, physical activity during cancer treatment can:
Pretty convincing!
But exercise doesn’t happen on paper and research alone isn’t always compelling - so here are some additional reasons to consider working out that are more rooted in the human spirit of making the most out of a bad situation.
How Working Out During Cancer Treatment Helped Me
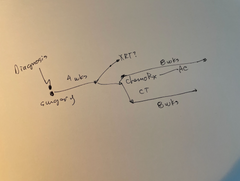
I’m a stage 4 melanoma patient and have gone through two diagnoses and immunotherapy treatments. Each time, I’ve found working out to be an integral part of getting through the insanity.
These explanations might be extensions or qualifications of what the research has distilled, but I think it’s worth explaining in human terms:
Working out allows you to set goals
Even if you can’t establish a workout routine like you had before treatment, it’s still a relatively controllable goal to move around in some capacity every day.
I know that checking the ‘worked out’ box off my short to-do list each day I could during treatment gave me a sense of fulfillment - especially as I believe it to be so healthy.
Sweating it out is cathartic
In the literal sense, it felt like I was sweating immunotherapy toxicity out of my body. Research shows that I likely was. Additionally, being able to push myself regularly - even if ‘pushing myself’ was walking up and down the block - let me distract myself and feel as though there was a pathway to improving my body.
Exercise can be social
I’m a runner and a basketball player primarily. While some treatments may leave you immunocompromised and not wanting to be around many people, if there is a chance to do group exercise, I highly encourage it.
Some days, when I could move as briskly, I did group yoga classes or went for a bike ride with a friend. Other times, I would do plank and pushup challenges asynchronously with my gym buddies.
Working out brings normalcy
Cancer is weird. Cancer treatment is weird. Most of the interactions from diagnosis through treatment and beyond are weird. Even if working out wasn’t your favorite thing to do before cancer, it’s a thing that non-cancer patients do.
When I was on a jog, shooting hoops, or lifting weights, it was an escape from the weird. I could relate to other people who weren’t cancer patients because we shared this part of everyday life still.
What Kind of Exercise Should You Do During Cancer Treatment?
It’s important to note that exercise during cancer treatment is not one-size-fits-all or a competition. The goal is to stay moving and engage in moderate aerobic exercise for 3-4 hours per week.
Depending on your fitness level before diagnosis and your energy level during treatment, consider trying these exercise options:
These are just a few suggestions; whatever way you can move around without risking injury is likely to benefit your mind and body. Be sure to ask your oncologist and any specialists assigned to your case if you have questions about the suitability of certain exercise types.
Dr. Blayney adds:
I agree with Mike that exercise can help in many parts of cancer and its treatment. When I recommended exercise to patients, I could see that many were put off by this recommendation, as they thought it would only add to their fatigue or sense of loss. I would always add “It doesn’t have to be NFL training camp type exercise. Start walking a few minutes each day. Walking 30 minutes daily or 140 minutes per week is enough”
Also, when well meaning friends recommend supplements, diets or other treatments, I suggest thanking them for their concern, and acknowledging their friendship and concern: “Thank you for your concern and love. My doctor recommends exercise. Can you help me with this commitment by meeting me for a walk each week?” I found that this suggestion made all parties feel better.
Why You Should Work Out During Cancer Treatment
Ultimately, getting a workout in during cancer treatment is both about the science and the feelings. We know it’s good for us as patients, and I believe it to be just as important to the human condition outside the clinical scope.
The goal of working out during cancer treatment isn’t to get jacked or make the Olympics, but I’ve found it helpful to maintain muscle mass and sanity. For these reasons among the well-researched medical ones, I encourage you to find time to break a sweat whenever you’ve got the energy to during treatment.
Related Articles:
Our team “gets it”
The Manta Cares team is composed of cancer survivors, caregivers and oncologists - so we truly understand the challenges that come with a cancer diagnosis because we’ve been there. We are here to walk with you as you go through your own cancer experience. Please don’t hesitate to reach out with any questions. Be sure to subscribe to our newsletter and check out our free resources like our Chemotherapy Checklist for Caregivers, Financial Checklist for Cancer Treatment and more. We also put out a bi-weekly podcast called the Patient from Hell to educate, empower and hopefully inspire you as you go through this crappy experience. You can listen on Spotify, Apple Podcasts, YouTube or anywhere you listen to podcasts. Dealing with cancer as a patient or caregiver can feel really lonely. Just know that you are not alone in this experience.
About the author: Mike Linn is a writer, athlete, business owner, and now a cancer patient advocate. He was first diagnosed with stage 3c metastatic melanoma at the age of 30 and had a stage 4 recurrence in 2023 at 35. In a better effort to understand the mental health side of being a cancer patient, he began posting content to social media and support groups and has yet to stop talking about his cancer experience both personally and professionally. Mike also loves candy and is determined to dispel the notion that sugar specifically feeds cancer - or he is at least hopeful that research will prove this.
Disclaimer: All content and information provided in connection with Manta Cares is solely intended for informational and educational purposes only. This content and information is not intended to be a substitute for medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.