Medically reviewed by Dr. Douglas Blayney, August 10, 2023

If you or your loved one is living with a life-threatening illness, it’s overwhelming to think about where to turn for support. Hearing the words “palliative care” can be scary, as people often equate palliative care to the end of life. But using palliative care does not mean you are giving up hope! Let’s look at the 5 stages of palliative care to see what they mean and how they can be supportive at all times during an illness for you and your loved one.
What is Palliative Care?
Palliative care focuses on providing comprehensive support to individuals facing life-threatening illnesses. Palliative care is directed to controlling symptoms. Palliative care is not the same as hospice care. Palliative care can be used at any point in the cancer experience often alongside curative treatments, and isn’t the same as “end of life” care. The primary objective of palliative care is to improve the quality of life for patients and their families by addressing physical, emotional, social, and spiritual needs.
What Is The Difference Between Primary and Secondary Palliative Care?
It may be helpful to think of primary palliative care and secondary palliative care. Primary palliative care is often provided by the oncologist, the primary treatment team, or a primary care physician. Examples include pain medication or anti-nausea medication provided as part of post operative care or with chemotherapy.
Secondary palliative care usually involves a palliative care specialist, and can include treatment of difficult to control pain or nausea, or specialized treatments for neuropathy, depression or other. Referral to a palliative care specialist does not mean that the oncology team is giving up or recommending giving up, anymore than referral to an endocrinologist or gynecologist is giving up – referral means the primary oncologist or team needs more sophisticated advice.
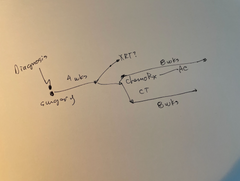
5 Stages of Palliative Care
We will explore the different stages of palliative care, highlighting the importance of a multidisciplinary approach to alleviate suffering and promote a sense of comfort and dignity for patients.
Stage 1: Assessment and Planning
The first stage of palliative care involves a thorough assessment of the patient's medical history, current health status, symptoms, and overall quality of life. A team of healthcare professionals, including doctors, nurses, social workers, and spiritual counselors, collaborates to gather comprehensive information. This multidisciplinary approach allows for a holistic understanding of the patient's needs and preferences.
Once the assessment is complete, an individualized care plan is developed, taking into account the patient's goals, values, and treatment preferences. Communication with the patient and their family is crucial during this stage, as it establishes trust and helps align care goals with the patient's desires. Effective communication and shared decision-making lay the foundation for a supportive and patient-centered approach.
Stage 2: Symptom Management
The second stage of palliative care focuses on symptom management. Patients facing life-threatening illnesses often experience a range of distressing symptoms, such as pain, nausea, fatigue, and anxiety. Palliative care specialists are experts at controlling and alleviating these symptoms, aiming to enhance the patient's comfort and well-being.
Pain management is often a primary focus during this stage. Palliative care teams employ a variety of techniques, including pharmacological interventions (prescription medications, often including narcotics), physical therapy, and non-pharmacologic therapies like acupuncture, to address pain effectively. Managing other distressing symptoms is also prioritized, ensuring that the patient's physical discomfort is minimized to the greatest extent possible.
Stage 3: Psychosocial Support
The third stage of palliative care emphasizes the provision of psychosocial support to patients and their families. Spiritual and religious counseling are an integral part of this support. A life-threatening illness can profoundly impact a patient's emotional well-being, leading to feelings of fear, sadness, or hopelessness. Palliative care specialists recognize the importance of addressing these emotional challenges to maintain a positive outlook on life and cope with the illness.
Social workers and counselors play a vital role in this stage, providing emotional support and counseling to both patients and their families. They assist in facilitating difficult conversations, addressing concerns about the future, and helping patients find meaning and purpose amid their illness. By fostering emotional resilience, palliative care helps patients and families navigate the challenges with greater strength and acceptance.
Stage 4: Communication and Shared Decision-Making
Effective communication is a cornerstone of palliative care, and the fourth stage centers on promoting open, honest, and compassionate dialogues between patients, families, and healthcare providers. As the patient's condition may change over time, ongoing communication is essential to adapt the care plan and treatment goals accordingly.
Palliative care teams encourage patients to express their values, goals, and preferences regarding their care. By understanding the patient's wishes, healthcare providers can ensure that medical decisions align with their goals for quality of life. This approach empowers patients to maintain control over their care, fostering a sense of autonomy and dignity in the face of illness.
Stage 5: End-of-Life Care
End-of-life care is when palliative care transitions to hospice care when there are no longer curative treatment options being offered to a patient. Hospice addresses the specific needs of patients, families and other caregivers in the patient’s last days, weeks, or months of life. Hospice strives to provide comfort and support during this challenging time, enabling patients to experience a peaceful and dignified end of life.
During end-of-life care, hospice care teams focus on alleviating pain and symptoms, promoting emotional well-being, and facilitating meaningful connections with loved ones. Spiritual counselors may offer guidance to patients and families seeking solace in their beliefs. Additionally, the hospice care team provides bereavement support to family members after the patient's passing, acknowledging the ongoing need for compassionate care during the grieving process.
Frequently Asked Questions about the 5 stages of Palliative Care
How Is Palliative Care Funded?
In the US, funding for palliative care typically involves a combination of sources:
- Private Insurance: Many private health insurance plans cover palliative care services as part of their benefits. Patients can use their insurance to cover consultations, medications, and treatments related to palliative care.
- Medicare: Medicare, a government-funded program that provides health coverage for people aged 65 and older, covers palliative care services under its hospice benefit. Hospice care, a specialized form of palliative care for patients with terminal illnesses, is funded through Medicare's hospice benefit.
- Medicaid: Medicaid, a joint federal and state program that provides health coverage for eligible low-income individuals, also covers palliative care services. States may have different rules and regulations for Medicaid coverage of palliative care.
- Out-of-Pocket Payments: Some patients and families may need to pay for palliative care services out of pocket, especially if they don't have insurance coverage or if certain services are not covered by their insurance.
- Non-Profit Organizations and Charities: Various non-profit organizations, hospice centers, and palliative care clinics rely on donations and charitable contributions to fund their services. These organizations often provide financial assistance to patients who cannot afford palliative care.
- Hospice Agencies: Hospice care, which is a specialized form of palliative care, is often provided by hospice agencies. These agencies may receive funding from a combination of Medicare reimbursements, private insurance, and charitable donations.
Read more: Cancer Journey: Setting Up Your Team
Read more: Cancer Financial Toxicity & Health Inequities with Rosie Cunningham of Family Reach
How Long Does Palliative Care Typically Last?
The duration of palliative care can vary widely depending on the individual patient's medical condition, needs, and goals of care. Palliative care is not limited by a specific timeframe and can be provided for as long as it is deemed beneficial to the patient's well-being and quality of life.
How Can Family And Friends Best Support A Patient In Palliative Care?
Support from family and friends is incredibly valuable for patients receiving palliative care. Here are some ways that family and friends can provide the best possible support:
- Open Communication: Maintain open and honest communication with the patient. Listen to their needs, concerns, and wishes, and encourage them to express their feelings and preferences about their care.
- Be Present: Spend time with the patient. Your presence can offer comfort and companionship. Just being there to talk, share stories, or simply sit quietly can make a positive impact.
- Respect Wishes: Respect the patient's wishes regarding their care and treatment decisions. This includes adhering to any advance directives, living wills, or other documents they may have prepared.
- Empathetic Listening: Be a good listener and offer emotional support. Let the patient express their emotions without judgment, and offer reassurance that their feelings are valid.
- Help with Practical Tasks: Offer assistance with practical tasks such as grocery shopping, cooking, cleaning, and running errands. These tasks can become challenging for the patient, and your help can make their daily life more manageable.
- Provide Respite: Caregiving can be demanding. Offer to provide respite care to the primary caregiver if the patient is being cared for at home. This can give the caregiver a break to rest and recharge.
- Create a Comfortable Environment: Ensure that the patient's living space is comfortable and conducive to their well-being. Consider their preferences for lighting, temperature, and decor.
- Offer Diversions: Engage in activities that the patient enjoys, such as watching movies, listening to music, reading books, or engaging in hobbies. These activities can provide moments of joy and distraction.
- Respect Privacy: Be mindful of the patient's need for privacy and personal space. Always ask for permission before sharing information about their health or situation.
- Be Sensitive: Be sensitive to the patient's energy levels and comfort. Sometimes they may need rest or solitude, so respect their need for space.
- Stay Educated: Educate yourself about the patient's medical condition, treatment options, and potential challenges. This will enable you to have informed discussions and provide better support.
- Offer Emotional Support: Palliative care can be emotionally taxing for both the patient and their loved ones. Offer emotional support and reassurance, and encourage them to seek professional counseling if needed.
- Practice Self-Care: Supporting a loved one in palliative care can be emotionally demanding. Make sure you also prioritize your own well-being and seek support for yourself if needed.
Remember that every patient's needs and preferences are unique, so it's important to have ongoing conversations with the patient and their primary caregivers to understand how you can provide the most meaningful and effective support.
Read more: Techniques to manage stress and uncertainty with professor and author Dr. Manuela Kogon (Part 2)
Where is Palliative Care Provided?
The choice of setting for palliative care depends on the patient's medical condition, preferences, and available resources. The healthcare team, along with the patient and their family, will work together to determine the most appropriate and supportive environment for receiving palliative care.
What Diseases Can Be Treated by Palliative Care?
Palliative care can be beneficial for individuals with a wide range of serious, chronic, or life-limiting illnesses. The primary focus of palliative care is to improve the quality of life for patients by managing symptoms, providing emotional and psychological support, and addressing the overall well-being of both the patient and their family. Some of the diseases and conditions that can be treated or managed through palliative care include: cancer, heart disease, neurological diseases, COPD, kidney disease, liver disease, HIV/AIDS, stroke, etc. The WHO has a comprehensive fact sheet on this as well, which you can read here.

Disclaimer: This blog post is for general informational purposes only and does not constitute the practice of medicine, nursing or other professional health care services, including the giving of medical advice, and no doctor/patient relationship is formed. The use of information on this blog or materials linked from this blog is at the user's own risk. The content of this blog post is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Users should not disregard, or delay in obtaining, medical advice for any medical condition they may have, and should seek the assistance of their health care professionals for any such conditions.