Medically reviewed by Dr. Doug Blayney on December 18, 2023
If you’re like me, you hear the word “mammogram” and cringe just a little bit. We’re going to demystify the mammogram, its purpose and the general experience for you. A mammogram is a special kind of x-ray that helps doctors check for any unusual changes in a woman's breast tissue. It's an important tool in finding breast cancer early. The mammogram depends on the contrast between fat in the normal breast tissue, the gland – milk producing – tissue, and any calcium deposits which may form. Mammograms are more accurate with more fatty tissue in the breast. It’s normal for fatty tissue to accumulate as women and men get older.
During a mammogram, a woman's breast is gently pressed to spread out the tissue between two flat plates to create detailed pictures of the inside. The process might feel a little uncomfortable, but it only lasts for a short time. I sometimes find that the anticipation of the mammogram is worse than the mammogram itself. Doctors recommend mammograms for women, especially those over 40, as a way to detect any potential signs of breast cancer early on. Early detection increases the chances of successful treatment and recovery. So, even though it might seem a bit inconvenient, getting a mammogram is a smart and proactive step in taking care of your health.
How is a mammogram performed?
While each medical office can have a slightly different process, here is a general list of things to expect when you go into have a mammogram:
- Check-In: When you arrive for a mammogram, you'll first check in at the reception desk. They'll ask you some questions and make sure all your information is correct.
- Changing clothes: After checking in, you'll be given a special gown to wear. It's important to wear this gown to make the mammogram process easier.
- Mammography room: A technician will guide you to the mammography room. They'll explain the process and answer any questions you might have.
- Breast compression: The technician will help position your breast on a flat platform. Another flat plate will press down gently to spread out the breast tissue. This might feel a bit tight, but it helps create clear X-ray pictures.
- X-ray pictures: The mammogram machine takes X-ray pictures of your breast from different angles. The process is quick, and you'll need to stay still for a few moments during each picture.
- Repeat for other breast: The same steps are repeated for the other breast, ensuring a thorough examination.
- Wait for results: After the mammogram, you might need to wait a bit for the results. The pictures will be carefully examined by a doctor to check for any signs of concern. A screening mammogram facility may not have a radiology doctor immediately available to interpret the results, and so the results may take a day or two and are usually delivered over the telephone or through a patient’s portal. Results of a diagnostic mammogram are usually available more quickly, in case additional views of the breast are needed.
- Follow-up, if needed: If the doctor finds anything unusual, they may recommend additional tests or follow-up appointments. It's important to follow their advice to ensure your health.
Overall, the entire mammogram process usually takes around 20-30 minutes. While it might feel a little uncomfortable during the compression, it's a vital step in taking care of your breast health.
Do mammograms hurt? What causes breast pain after a mammogram?
Feeling discomfort during a mammogram is normal for some people because the machine needs to press the breast to take clear pictures. The discomfort is temporary, and the mammogram is an important test to help find any potential breast issues early. Some factors that might impact your discomfort are:
- Breast Size: Larger breasts may experience more pressure and discomfort during a mammogram because there is more tissue to compress. The compression is necessary to obtain clear images, but it can contribute to temporary discomfort, especially for women with larger breasts.
- Menstrual Cycle Timing: Breast tenderness and sensitivity can vary throughout the menstrual cycle. Some women may experience more discomfort or pain during a mammogram if it coincides with the days leading up to their menstrual period when breasts tend to be more sensitive. It's advisable to schedule the mammogram during a time when breast tenderness is likely to be lower.
- Variations in Positioning: The positioning of the breast during a mammogram can influence the level of discomfort. Different angles and positions are necessary to capture images from various perspectives. The mammographer will work to position the breast correctly for the best imaging results, and this positioning may cause temporary discomfort.
- Mammographer’s Skill: The skill and experience of the mammographer play a crucial role in the level of discomfort during a mammogram. A skilled mammographer understands how to position the breast optimally, minimizing discomfort while ensuring the quality of the images. Choosing a qualified and experienced professional can contribute to a more comfortable and effective mammogram experience.
It's important to communicate openly with the mammography technologist and radiology doctor about any concerns or discomfort. They can provide guidance on ways to enhance comfort and make adjustments to the procedure as needed. After a mammogram, your breasts might feel sore for a short time, usually just a day or two, but the discomfort is temporary. If your breast is sore after mammogram and the pain persists, be sure to call your healthcare provider.
Read more: 6 Types of Cancer Specialists
Tips to minimize pain during mammogram
You might be wondering how to alleviate breast pain after a mammogram. Here are some tips to minimize the discomfort of a mammogram. Be sure to ask your health care team for recommendations, too:
- Schedule smart: Plan your mammogram appointment one to two weeks after your period to minimize breast tenderness caused by hormonal changes.
- Take a pain reliever: Consider taking an over-the-counter painkiller 45 to 60 minutes before your mammogram to help reduce any discomfort during the procedure.
- Speak up: Communicate openly with your mammographer about your pain tolerance or any chronic pain conditions you may have. They can tailor the screening to make it as comfortable as possible for you.
- Watch your salt intake: Reduce salty foods in your diet before the mammogram, as salt can cause water retention, making breast compression more uncomfortable.
- Cut back on caffeine: Avoid or reduce caffeine intake from coffee, tea, and soft drinks one to two weeks before your mammogram, as it can contribute to breast tenderness.
- Relaxation techniques: Practice breathing exercises and meditation before your mammogram to help relax your body and reduce tension, making the experience less uncomfortable.
By incorporating these strategies, you can take proactive steps to make your mammogram as comfortable as possible while still ensuring a thorough and effective screening.
Write down notes and questions to review with your doctor using our Manta Planner or Notebook.
When to see your healthcare provider
A mass in your breast or a discoloration in the skin over the breast, which persists for longer than one month or over one menstrual cycle is a cause for concern. Usually these findings do not represent cancer, but if they do not completely go away, you should seek advice from your healthcare provider. Often a mammogram is a first step in evaluating a mass and determining if further tests are needed. A mass that doesn’t go away, even if a mammogram is normal, should trigger further testing, which may include an ultrasound, a breast MRI, or a biopsy.
Getting a mammogram is important for normal women to check for any changes in their breasts which may not be detected by self examination or a physician’s examination. Healthcare providers usually recommend women start getting mammograms around the age of 40, and it's a routine part of taking care of their health. In May 2023, the U.S. Preventive Services Task Force revised its recommendations, lowering the recommended starting age for mammograms from 50 to 40. For those at a higher risk, such as those with a family history of breast cancer, doctors may suggest starting mammograms earlier or having them more often. High-risk individuals might also benefit from additional screenings, like breast sonograms or MRIs, to get a more detailed look at the breast tissue.
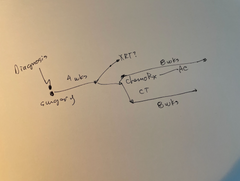
Sometimes, after a mammogram, healthcare providers might recommend a second mammogram, a breast sonogram, or a biopsy to learn more about any unusual findings. A second mammogram might be needed if the images aren't clear, while a breast sonogram uses sound waves to create detailed pictures. A biopsy involves taking a small sample of breast tissue to examine it closely. These additional tests help doctors gather more information and make the best decisions for a person's health. It's essential to follow the advice of healthcare providers to ensure early detection and effective management of any potential breast health concerns.
When to schedule a mammogram
When planning a mammogram, it's a good idea to think about a few things. First, try not to schedule it during your period when your breasts might be more sensitive. Healthcare providers usually recommend women start getting mammograms around the age of 40, and it's a routine part of taking care of their health. According to the American Cancer Society for women at average risk for breast cancer:
- Women between 40 and 44 have the option to start screening with a mammogram every year.
- Women 45 to 54 should get mammograms every year.
- Women 55 and older can switch to a mammogram every other year, or they can choose to continue yearly mammograms. Screening should continue as long as a woman is in good health and is expected to live at least 10 more years.
For women at higher risk for breast cancer, the American Cancer Society recommends a breast MRI and a mammogram every year, typically starting at age 30. This includes women who:
- Risk of breast cancer is estimated to be 20% to 25% or more throughout their lifetime. This estimation is often done using tools that look at family history. (Ask your healthcare provider about assessment tools)
- Knows they have a BRCA1 or BRCA2 gene mutation based on genetic testing
- Women with a first-degree relative (like a parent, brother, sister, or child) who has a BRCA1 or BRCA2 gene mutation, but haven't had genetic testing themselves
- Received radiation therapy to the chest between the ages of 10 and 30, they are at higher risk
- Women with certain syndromes like Li-Fraumeni, Cowden, or Bannayan-Riley-Ruvalcaba, or if their first-degree relatives have these syndromes, should also have yearly screenings.
For more information about breast cancer surveillance screening, listen to our Patient from Hell podcast “Episode 40: Navigating Breast Cancer Survivorship” with Karen Wernli, PhD.
FAQs
How long does a mammogram take?
A mammogram usually takes about 20 to 30 minutes from start to finish. It's a quick and important checkup that helps doctors see inside your breasts to make sure everything is healthy.
What are the side effects of mammograms?
Mammograms generally do not have serious side effects, but some people may feel temporary discomfort or mild pain during the procedure when the breasts are pressed. This discomfort usually goes away quickly, and the benefits of detecting potential breast issues early outweigh any brief discomfort.
What to do if a mammogram is too painful?
If a mammogram is too painful, it's important to let the technologist know right away. They can make adjustments to ensure you are as comfortable as possible during the procedure, and discussing any concerns can help make the experience more bearable.
Is it normal to have breast pain after a mammogram?
It's normal for some people to experience temporary breast discomfort after a mammogram due to the pressure applied during the procedure. This pain is usually mild and short-lived, but if it persists or becomes severe, it's important to contact your healthcare provider for guidance.
If I have a mass that I can feel, and my mammogram is normal, what do I do?
If the mass does not completely resolve, then further testing – which may include ultrasound of the breast, MRI of the breast, or a biopsy of the mass – may be necessary.
Disclaimer: The content provided by Manta Cares Inc. is intended for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website.
While we strive to keep the information up to date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the website or the information, products, services, or related graphics contained on the website for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
The use of our platform does not create a doctor-patient relationship. Manta Cares Inc. does not recommend or endorse any specific tests, physicians, procedures, opinions, or other information that may be mentioned on the site. Reliance on any information provided by Manta Cares Inc., Manta Cares Inc. employees, others appearing on the site at the invitation of Manta Cares Inc., or other visitors to the site is solely at your own risk.
The site may contain health- or medical-related materials that are sexually explicit. If you find these materials offensive, you may not want to use our site. The site and the content are provided on an "as is" basis.