Medically reviewed by Dr. Doug Blayney on April 8, 2024
Introduction
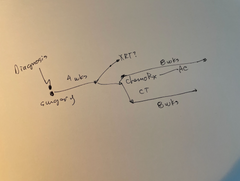
Breast cancer patients have different options for surgery, including mastectomies and lumpectomies. Mastectomies involve removing the entire breast, while lumpectomies remove only the tumor and surrounding tissue, leaving the breast intact. Understanding these options is crucial for breast cancer patients because it allows us to make informed decisions about our treatment. Some of us may choose mastectomy for various reasons, such as reducing the risk of cancer recurrence, while others may prefer lumpectomy to preserve their breast. Knowing the types of surgery available helps you work with your healthcare team to choose the best option based on your individual medical needs (or that of your loved one), preferences, and personal circumstances. Knowing your options and being able to discuss those decisions with your care team will empower you to take an active role in your treatment and helps ensure you or your loved one will receive the most appropriate care for your specific situation.
I had a bilateral mastectomy in 2011 and will speak to some of the questions I am often asked as well as questions we get within our Manta Cares community of cancer patients, caregivers and survivors. Keep in mind that every person’s situation is a little different, so make sure you ask your doctor and care team what makes the most sense for you. If you need help remembering questions to ask before your appointment, take a look at our Manta Planner. You can take notes, write down questions or concerns and not worry that you’re going to forget your list while you’re actually in the appointment (which is something I say from personal experience… I always remembered the questions I meant to ask about ten minutes after my appointment ended… doh!).
The Basics of Mastectomy
I’ll be honest, before I was diagnosed with breast cancer I didn’t know what a mastectomy was. In fact, there were a lot of cancer words that sounded like another language to me when I was dropped into “Cancerland”. We will give you an overview on mastectomies below.
What is a Mastectomy?
A mastectomy is a surgery where doctors remove one or both breasts. This procedure is often done to treat breast cancer or to prevent it from spreading. During a mastectomy, surgeons cut through the skin and tissue of the breast to remove the breast tissue, sometimes including the nipple and areola. After the surgery, some people may choose to have breast reconstruction surgery to rebuild the shape of the breast. Mastectomies can help stop the spread of breast cancer and reduce the risk of it coming back.
Types of Mastectomies
There are a number of different types of mastectomies including:
- Simple Mastectomy and Modified Radical Mastectomy: These terms are often used interchangeably. Removes the entire breast tissue but leaves the chest muscles untouched. It's usually done when cancer hasn't spread to the skin over the breast tissue or deep into the chest wall. If reconstruction with an implant, a tissue expander is often put in place during the surgery.
- Radical Mastectomy: Removes the entire breast, chest muscles, and lymph nodes under the arm. It's less common now and usually only used in rare cases.
- Skin-Sparing Mastectomy: Removes breast tissue but keeps most of the skin, making it easier for breast reconstruction surgery afterward. A tissue expander is often put in place with this surgery as well.
- Nipple-Sparing Mastectomy: Removes breast tissue while keeping the nipple and areola intact. It's usually done when cancer hasn't spread to the nipple, and often done in stages (that is two operations) in order to preserve the blood flow to the nipple and keep it alive. Tissue expanders are often placed during one of the surgeries in this technique.
- Double Mastectomy: Removes both breasts, sometimes done to prevent cancer or treat it in both breasts. It's a personal choice and can reduce the risk of future cancer in individuals who are at high risk for cancer in the opposite breast, such as those with certain genetic mutations. Again, tissue expanders may be part of the surgeries as well.
Why Mastectomy Might Be Necessary
A mastectomy might be necessary for different reasons, mainly when treating breast cancer. If cancer has spread throughout the breast or is in several areas, removing the entire breast through mastectomy may be needed to stop its spread. Additionally, some patients with a high risk of breast cancer due to genetic factors or previous treatments may choose to have a mastectomy as a preventive measure. Benefits of a mastectomy, compared with a lumpectomy, depend on factors like the stage and type of cancer, the size of the cancer in relation to the size of the breast, and the number of cancer deposits in the breast, overall health, and personal preferences. It's important for patients to discuss with their doctors to understand if mastectomy is the best option for them based on their individual circumstances.
Also Read: How to Sleep After a Mastectomy
Understanding Sensation Loss
I think most of us have a tendency to not realize how important working body parts are until they no longer work like they should. I always took for granted I had full sensation of my chest. I don’t think I ever really noticed it… except maybe when I had a bruise or some other painful (temporary!) reminder of that area. Until my mastectomies robbed that area of most sensation. Then all of a sudden, it became very apparent that something was missing. Sometimes it literally just felt like a dead zone - I could feel pressure but not sensation. At first that was very jarring, but now, twelve years later, it’s all I remember. It always amazes me how much we adapt to new situations… especially when forced to!
The Nerve Network of the Breast
Understanding sensation loss after a mastectomy starts with knowing the nerve network of the breast. Nerves run through the breast tissue, sending messages to the brain about touch, temperature, and pain. This network helps us feel sensations in our breasts, including during activities like hugging or wearing clothing. When someone has a mastectomy, these nerves can be damaged or removed along with the breast tissue, leading to a loss of sensation.
Why Sensation Loss Occurs
Sensation loss after mastectomy happens because surgical procedures disrupt the nerve endings in the breast. During mastectomy, surgeons may need to cut through or remove nerves to remove the breast tissue effectively. Additionally, the removal of lymph nodes under the arm can also impact nearby nerves, leading to further sensation loss. While some sensation may return over time as nerves heal, it's common for patients to experience permanent changes in sensation after mastectomy. This loss of sensation can affect how the breast and surrounding area feel to touch, impacting everyday activities and body image.
The Emotional and Physical Impact
In addition to the physical loss of sensation, there is also an emotional part of dealing with cancer and everything that goes along with it. Cancer, the gift that keeps on giving, right?!
How Can the Loss of Breast Sensation Impact Women?
The loss of breast sensation after a mastectomy can have a significant impact on women's lives. Beyond the physical aspect, sensation loss can affect how women feel about their bodies and themselves. Many women report feeling a sense of disconnection from their bodies or a loss of femininity due to the changes in sensation. This can lead to feelings of sadness, frustration, or even grief over the loss of a part of their identity.
Beyond the Physical Loss
Emotionally, the sensation loss can also contribute to anxiety and depression for some women. They may struggle with feelings of self-consciousness or insecurity, especially during intimate moments or when wearing certain clothing. The loss of sensation can make it challenging to feel comfortable in their own skin and may affect their relationships and overall quality of life. Additionally, the emotional impact of sensation loss can persist long after the physical recovery from surgery, requiring ongoing support and coping strategies.
The Importance of Sensation to Survivors
For breast cancer survivors, sensation loss underscores the importance of finding alternative sources of comfort and connection. While the physical sensation may be gone, we can still find ways to feel empowered and confident in our bodies. I will also add that now that I’m 12 years out from my double mastectomy, I honestly can’t remember how things use to work and feel. You really do adapt to your “new normal” – I wouldn’t have necessarily chosen this “boob amputation” as I sometimes call it, but we really do adapt and “do what we’ve gotta do” to keep moving forward. I’ve found that seeking support from loved ones and support groups of other women who have been through breast cancer has been incredibly healing for me.
Innovations in Restoring Sensation
Is there an answer to the nerve damage that gives many of us breast cancer survivors a loss of sensation in the chest area? This was not even discussed with me twelve years ago, and now there are newer surgical techniques that might help with at least some of this loss.
Can Breast Reconstruction Restore the Sensation?
Breast reconstruction surgery can restore the appearance of the breast after a mastectomy, but it usually cannot fully restore sensation. While some techniques, like nerve-sparing surgeries, aim to preserve nerve function and potentially maintain some sensation, the nerves that are removed during mastectomy cannot be completely replaced. However, advances in surgical techniques and research continue to explore ways to improve outcomes and potentially restore sensation for some women undergoing breast reconstruction. It's important for you to discuss your expectations and concerns with your healthcare team to understand the potential outcomes of breast reconstruction surgery fully.
Emerging Surgical Techniques
Emerging surgical techniques aim to address nerve damage after a mastectomy and potentially restore sensation to the breast area. One innovative method is breast reinnervation, which involves reconnecting nerves in the chest wall to nerves in the remaining breast tissue. This procedure aims to improve sensation in the breast area and may be performed alongside breast reconstruction surgery. A 2022 study review published in the Journal of the American Society of Plastic Surgeons looking back at 19 past studies on cadavers (sorry for the mental picture there!) identified “the most important nerves to spare or repair during reconstructive and cosmetic breast surgery.” They also commented that, “Future studies are required to elicit the course of dominant nerves through the breast tissue.” Other techniques, such as sensory re-education exercises and nerve grafting, are also being explored to help restore feeling in the breast area after mastectomy. While these techniques are still in the early stages of development, they hold promise for improving the quality of life for breast cancer survivors by addressing sensation loss after mastectomy.
Manta Care's Comprehensive Support System
Our team is made up of cancer survivors, caregivers and patients. So we get it!
Empowering Caregivers and Patients
We are here to walk with you as you go through your own cancer experience. Please don’t hesitate to reach out with any questions. Be sure to subscribe to our newsletter and check out our free resources like our Chemotherapy Checklist for Caregivers, Financial Checklist for Cancer Treatment and more. We also put out a bi-weekly podcast called the Patient from Hell to educate, empower and hopefully inspire you as you go through this crappy experience. You can listen on Spotify, Apple Podcasts, YouTube or anywhere you listen to podcasts. Dealing with cancer as a patient or caregiver can feel really lonely. Just know that you are not alone in this experience.
Conclusion
In conclusion, understanding the options available for breast cancer surgery, such as mastectomies and lumpectomies, is essential to make informed decisions about your treatment journey (or that of your loved one!). Each type of surgery has its benefits and considerations, and knowing the differences empowers you to work with you healthcare team to choose the best option for your needs. Whether opting for mastectomy to treat cancer or preserve breast health, or choosing lumpectomy to retain breast tissue, having info about these options enables you to take an active role in your care and ensure you receive the most appropriate treatment for you.
Navigating the emotional and physical impact of mastectomy involves recognizing the significance of sensation loss and its effects on overall well-being. Beyond the physical changes, sensation loss can lead to feelings of disconnection, sadness, and insecurity, impacting body image and emotional health. However, breast cancer survivors can find support and resilience in adapting to their "new normal" by seeking alternative sources of comfort and connection. There are also emerging surgical techniques that offer hope for restoring sensation after mastectomy, highlighting the importance of ongoing research to help improve outcomes and quality of life for breast cancer survivors.
FAQs
Who is eligible for breast reinnervation surgery?
Eligibility for breast reinnervation surgery depends on factors like the type of mastectomy and individual health conditions. Generally, it's considered for women who've had a mastectomy and are interested in restoring sensation to the breast.
How long will it take for sensation to return?
The time it takes for sensation to return after breast reinnervation surgery varies from person to person. Some may start feeling sensation within a few months, while for others, it may take longer.
Does the procedure require a long hospital stay?
Breast reinnervation surgery typically doesn't require a long hospital stay, usually just a day or two, unless there are complications.
What are the benefits of breast reinnervation?
Benefits of breast reinnervation surgery may include improved body image, enhanced psychological well-being, and a more natural feeling in the reconstructed breast.
How can I regain my sensation after mastectomy?
Regaining sensation after mastectomy can involve techniques like breast reinnervation surgery, nerve grafting, or sensory re-education exercises to help restore feeling to the breast area.
Do you lose feeling in your breast after mastectomy?
Yes, it's common to lose feeling in the breast after mastectomy due to damage to nerves during surgery.
Why do I have a lost sensation in my breast?
Lost sensation in the breast can occur due to nerve damage during mastectomy surgery, but it may be temporary and might improve over time.
Do you ever feel normal after a mastectomy?
While it's normal to experience changes after mastectomy, many people adapt and eventually feel normal again, especially with time and support. 12 years after my own bilateral mastectomy, I honestly don’t remember how things felt “before” – it’s amazing how the body and mind adapt to your new circumstances!
Underarm numbness after mastectomy?
Underarm numbness after mastectomy can occur due to nerve damage during surgery, but it may improve over time as nerves heal.
Why am I losing sensation in my nipples?
Loss of sensation in the nipples can happen after mastectomy due to nerve damage, but techniques like breast reinnervation surgery may help restore feeling.
Why is there no feeling in breast skin?
The lack of feeling in breast skin can result from nerve damage during mastectomy, but sensation-preserving techniques like nerve-sparing surgery can help minimize this.
What is a sensation preserving mastectomy?
A sensation-preserving mastectomy aims to minimize nerve damage during surgery, preserving feeling in the breast as much as possible.
How to relieve nerve pain after mastectomy?
To relieve nerve pain after mastectomy, treatments may include medications, physical therapy, or nerve blocks to manage discomfort. Talk with your care team to determine what makes the most sense for you.
Restoring sensation after mastectomy?
Restoring sensation after mastectomy can involve techniques like breast reinnervation surgery or sensory re-education exercises to help regain feeling in the breast area.
Do nipples lose sensitivity with age?
Nipples may lose sensitivity with age, but the degree of sensitivity varies from person to person.
What sensation is lost after mastectomy?
After mastectomy, sensations like touch and temperature may be lost in the breast area due to nerve damage during surgery.
Do nerves grow back after mastectomy?
While nerves don't regenerate fully after mastectomy, some regeneration may occur over time, leading to partial restoration of sensation.
What are the long term side effects of mastectomy?
Long-term side effects of mastectomy can include changes in sensation, arm and shoulder mobility issues, and emotional adjustments.
What are zingers after mastectomy?
Zingers, or sharp shooting pains, can occur after mastectomy due to nerve damage and are typically temporary.
Are muscles cut during mastectomy?
Muscles aren't usually cut during mastectomy, but tissue around the breast may be removed depending on the type of surgery.
Can you get a boob job after a mastectomy?
Yes, breast reconstruction, including breast implants or flap reconstruction, can be performed after mastectomy to restore breast volume.
Why do I feel tight after mastectomy?
Tightness after mastectomy can result from scar tissue formation or changes in tissue elasticity but usually improves over time. Check with your care team to see if physical therapy makes sense for you.
What I wish I knew before mastectomy?
This article covers a lot of the things I wish I’d known before my own bilateral mastectomy, but I’d also recommend finding others who have experienced this to talk to. Get their thoughts, tips and advice, but remember, every experience is unique, so you may run into different challenges during your own experience (or that of your loved one). Don’t be afraid to ask for help to navigate through the cancer experience – both physically and emotionally!
Disclaimer: The content provided by Manta Cares Inc. is intended for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website.
While we strive to keep the information up to date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the website or the information, products, services, or related graphics contained on the website for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
The use of our platform does not create a doctor-patient relationship. Manta Cares Inc. does not recommend or endorse any specific tests, physicians, procedures, opinions, or other information that may be mentioned on the site. Reliance on any information provided by Manta Cares Inc., Manta Cares Inc. employees, others appearing on the site at the invitation of Manta Cares Inc., or other visitors to the site is solely at your own risk.
The site may contain health- or medical-related materials that are sexually explicit. If you find these materials offensive, you may not want to use our site. The site and the content are provided on an "as is" basis.